A recent column in Med Page Today by David Nash draws attention to the frustrating issue of the quality measure development process (as well as its funding model). If any wound care practitioner has looked at their Quality and Resource Use Report (QRUR), you might have gotten a shock. I’ve been unsuccessfully trying to raise the alarm about the fact that wound care practitioners are being held accountable for hospital admissions and readmissions.
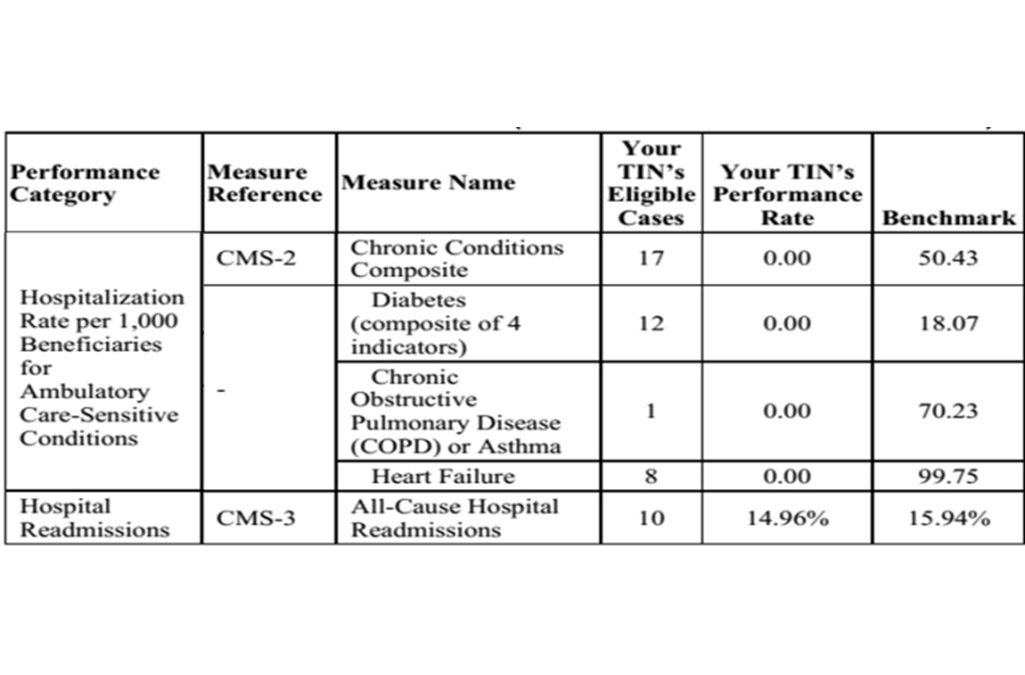
According to CMS data, In 2016, Medicare determined that 17 of my patients with chronic conditions were hospitalized as were 12 diabetic patients, 1 COPD patient, and 8 heart failure patients. You can see what my report looks like above.
If I had hit 20 in any of those categories, I could have had a claw back of money under PQRS. MIPS is working exactly the same way, only the stakes are higher. Keep in mind that I work less than half-time as a physician (2 days a week), yet my hospitalization rate was more than 50% of the threshold in two categories and was nearly half the threshold in a third. It’s safe to say if I had worked full-time in 2016, more than 20 patients would have been hospitalized in at least 2 if not 3 of the categories that comprise hospitalization rates per 1,000 beneficiaries for ambulatory care-sensitive conditions. Additionally, I was right at the halfway mark for “All Cause” hospital readmissions. The numbers make perfect sense if you know the prevalence rate of serious co-morbid conditions in my patients (60% with diabetes, 54% with ischemic heart disease, 24% with CHF, etc.). Tie those threads together: 24% of my wound center patients have CHF, and 8 of them got admitted to the hospital (most of them were also re-admitted). CMS says their admissions are “on me.” Similarly 54% of my patients have ischemic heart disease, and they contributed to my readmission rate, to say nothing of the fact that 60% of my patients have diabetes, and 12 of them got admitted for a variety of issues. I want to emphasize that most of the time, THESE ADMISSIONS USUALLY HAVE NOTHING TO DO WITH THEIR WOUNDS DIRECTLY. We are responsible for their admission and readmission FOR ANY REASON, by virtue of the fact that we provide the plurality of visits (unless you have a taxonomy to tell CMS that you are not the PCP).
The Hospital Readmissions Reduction Program (HRRP) was designed to reduce preventable hospital readmissions among Medicare beneficiaries by penalizing hospitals with higher-than-anticipated 30-day risk-adjusted readmission rates for targeted conditions, particularly acute myocardial infarction, heart failure, and pneumonia. While readmission rates might have declined since the HRRP was implemented, it’s not clear if it has improved care. What I CAN say is that this measure jeopardizes wound care practitioners. Because in 2016 there was no “taxonomy” by which I could explain to CMS that I am NOT the primary care physician (PCP) for these patients, and because I am board certified in Family Practice, and because I provided the plurality of services that year (wound center practitioners see these patients more often than their PCP), CMS assumes I AM the PCP. As an aside, that is why I changed my taxonomy to Hyperbaric medicine. At least it MIGHT indicate I am not the PCP. For more information and how it looks to change your taxonomy, click here. Later we can discuss why doing this still might not be enough.
If you are an internist or family practice physician who practices wound care, you are going to own the admissions and readmissions of every patient in the wound center. You could end up with monetary claw-backs under MIPS as a result, but that’s not the real problem. The worst of it is that you will end up with a low quality rating under MIPS, and that threatens your compensation rate, your negotiating position with payers, and your ability to stay on the panels of Accountable Care Organizations and preferred provider plans. This is a big deal folks.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos



What if it you had to admit a patient on his first visit to your clinic? How can you be held responsible for that?