Dear Manufacturer of Cellular and/or Tissue-based Products (CTPs) — commonly known as “skin substitutes”:
I feel compelled to explain the math of using CTPs in the hospital-based outpatient department (HOPD). A friend who is a podiatrist just told me about the latest product that he is using, and I told him, “Please do not send the rep to see me because I cannot use it.” She showed up 45 minutes later with promotional materials. The reason I can’t use the products that my podiatry colleagues are using is “package pricing.” I know you have heard of package pricing, but I’m going to explain it with numbers.
- If a product is in the “high tier,” then the reimbursement for the hospital is about $1,500 (I’m using round numbers) for the entire service of providing the CTP (including the cost of the product).
- It’s actually a bit less than that for us in Houston, because our wage index is less than 1.0.
- Medicare pays 80% of that amount, so what I am certain to get paid is $1,200.
- Not every patient has secondary insurance and I cannot make financial decisions that only work if the hospital ever gets the patient-responsible portion.
- That means, in the HOPD, $1,200 must purchase the CTP AND cover the cost of the staff, supplies, the clinic overhead, and the dressing we put over it (which might include an expensive compression bandage and expensive advanced dressing).
- It seems only reasonable for the hospital to want to “keep” at least $200 in order to pay the salaries of the clinic staff and the supplies (the dressing alone could be more than $30).
- That means that if the hospital pays more than $1,000 for the product itself, it runs the risk of losing money under package pricing.
When I assess which product I am going to use in the high tier, the first question I ask is, “Does it cost $1,000 or less?” The product that my podiatrist friend was using cost $10,000! He can use it because in his private office setting, he is paid the Average Sales Price (ASP) + 6%. That means my podiatrist colleagues can use any product that Medicare pays for, but I cannot.
If a product is low tier, I go through the same mental process with different numbers. That’s a total payment of about $500, of which I am certain to see 80% or $400, and if the hospital is to keep $200 (since the overhead, staff and supplies cost the same no matter what the “tier” of CTP), then the hospital can only afford a low tier product of about $200 or less.
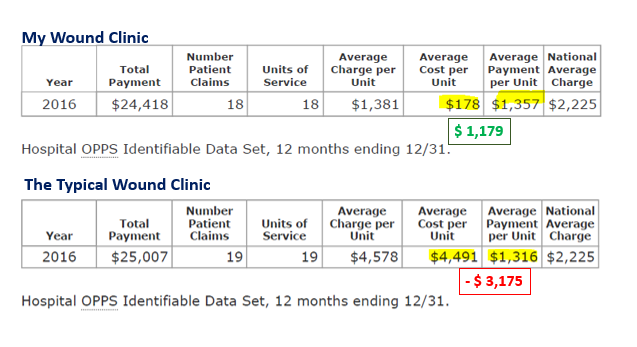
The hospital should not have to lose money to provide CTPs to patients, but most hospitals DO. You know how I know? I licensed a dataset (from American Hospital Directory) that provides cost and charge data by hospital for outpatient services. The chart above shows data from 2016 (although subsequent years only change with regard to volume). With regard to “skin subs,” you can clearly see the difference between my clinic, where I will not use a CTP if it means the hospital will lose money under package pricing, and a clinic I picked at random. Most wound centers look like the “Typical Wound Clinic.” In other words, most wound centers are LOSING THOUSANDS OF DOLLARS per application of a cellular product.
I don’t think my hospital should have to lose money to provide CTPs to patients, and I have been happy to offer that input when the hospital is negotiating contracts. There are a LOT of CTPs on the market. I might also add that your CTPs vary in price from about $30 per cm2 to $700 per cm2. If your product is 20x more expensive than another valid choice, you will need to show me that it’s 20x better.
I hope this provides some insight into why my first question is NOT about your clinical data, but your PRICE.
–Caroline
P.S. Next time, I will tell you what is going on with regard to CTPs and Medicare Advantage. One day I might discuss the average surface area of wounds that need CTPs — which has implications for products that are the size of a dime. And one day if I am really brave, I will write about the effectiveness of CTPs in the real world.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos



I am the Director of Coding and Reimbursement for a vertically integrated biologics company and I cannot tell you how many times a day I review this with hospitals that are stuck in sole or dual source GPO contracts. THANK YOU for writing this.CMS actually publishes the calculations for APC codes (5054 for skin graft applications) which is how the HOPD wound care center is paid.