This is a retired physician in his 90’s whose mind is as sharp as a tack. He’s got congestive heart failure (CHF) and leg edema so severe that his skin is splitting open. He’s a chair sleeper in part because he has orthopnea (shortness of breath lying down), but also because he has rest pain (pain in his feet with elevation that resolves with dependency). He’s old enough to have peripheral arterial disease (PAD) and given his complaint of rest pain, I can’t put his legs in compression without knowing that his arterial supply is adequate.
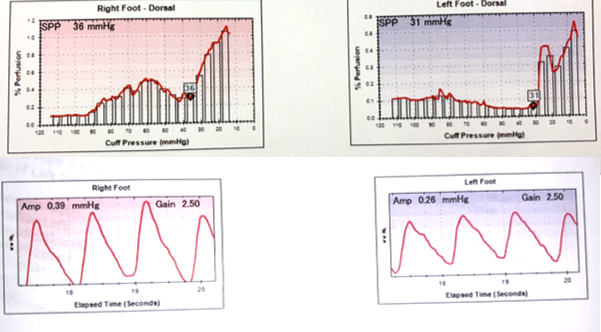
This is why I love my skin perfusion pressure (SPP) machine. The results of his SPP are fascinating. His SPP is in the low 30’s on both feet which is abnormally low (40 would be normal). That’s low enough to suspect PAD, but the pulse volume recording (PVR) of the feet is normal. In other words, there’s no evidence that the arteries are blocked. How could he have poor perfusion to his feet if his arteries are open? You guessed it – his cardiac ejection fraction is so low that his pump can’t send the blood to his feet! Once again, SPP told us something Arterial Doppler could not.
I decided to use Coban™ 2 Lite – which is only 20 mmHg of low stretch compression. That’s my “go to” option for patients with marginal perfusion. Remember that thanks to my SPP machine, I can know exactly what the perfusion pressure is, and as long as it’s well above 20 mmHg, I can give Coban 2 Lite a try – particularly if the patient is mentally alert and can take it off if it hurts. I don’t put patients in compression unless I KNOW their perfusion pressure.
Now for the rest of the story. When I first saw him, he would scream in pain when his legs were moved, he was depressed and generally miserable. Although his albumin was normal, his Vitamin D-OH was only 31. I got him to start taking 8,000 units of Vitamin D3 a day, and I started him on Juven, 2 packs a day (Juven® | Therapeutic Nutrition Powder). He tolerated gentle compression with Coban 2 Lite, and after about 4 months, not only were his ulcers healed, but his shortness of breath was improved, he was starting to ambulate, and he was also not depressed! He was like a different person. All I did was some gentle compression and nutritional supplementation, and it changed his life in a way that these photos can’t depict. I can’t be a wound care doctor without SPP and nutritional supplements.


Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos




Absolutely amazing