It’s a poorly kept secret that audits of wound care services rendered under the Medicare fee-for-service payment system are so pervasive that I don’t know anyone who is NOT in an audit of some kind. The entire alphabet soup of auditing bodies are at work: TPE, pre-payment, post-payment, RAC, ZPIC and even some I haven’t heard of before. What surprises me is that when I mention this, many hospitals shrug their shoulders and act like paybacks from audits are just the price of doing business. However, it does not seem like the situation is “business as usual” to me.
Since it’s not possible to prevent an audit, the only thing you can do is generate records that will protect you from recoupment. It takes more time and attention to do it right the first time than it does to respond to an audit. However, I suppose since clinicians are not usually the people who have to respond to an audit, the pain of an audit is felt by someone other than the person who created the documentation. And as long as the check for the money paid back is written by the hospital, physicians may not feel like it is their problem. Of course, if the physician is in a private office setting (where many wound care services are moving), that’s a different story. One physician told me that his practice had paid back 100% of their Medicare FFS payments for cellular and/or tissue-based products (CTPs) in an audit due to poor documentation. Their response was to stop using CTPs — not to fix their documentation issue.
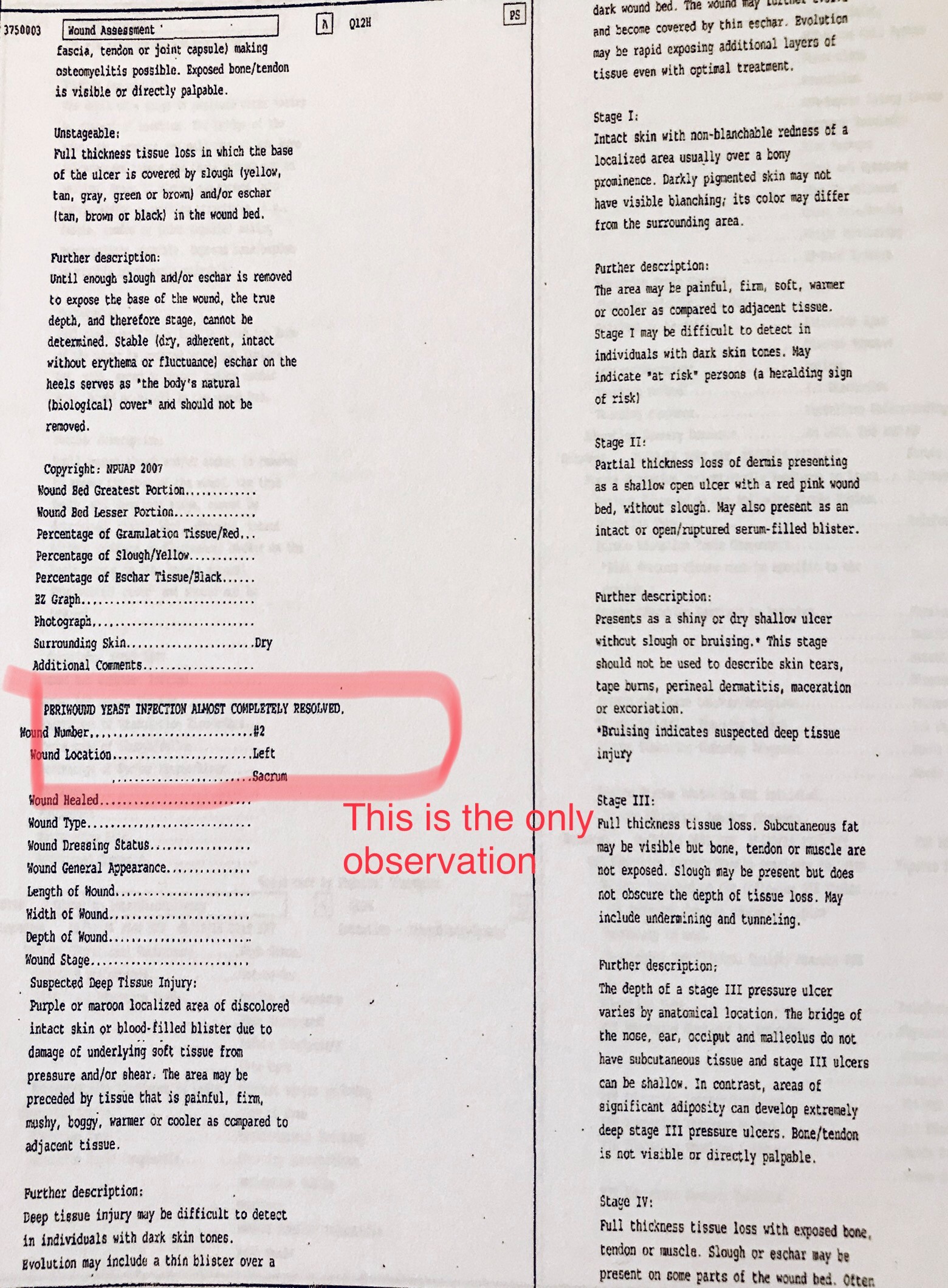
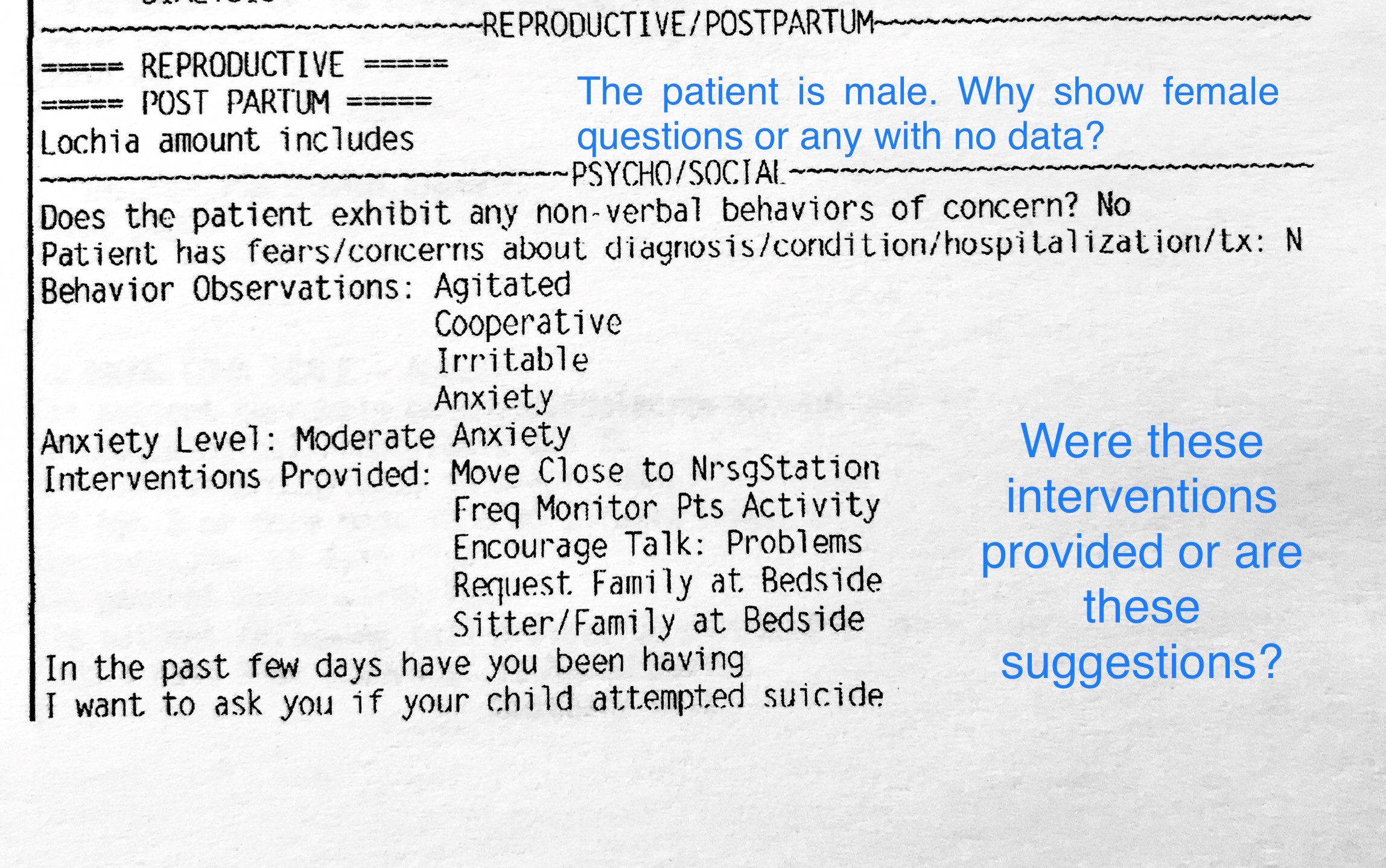
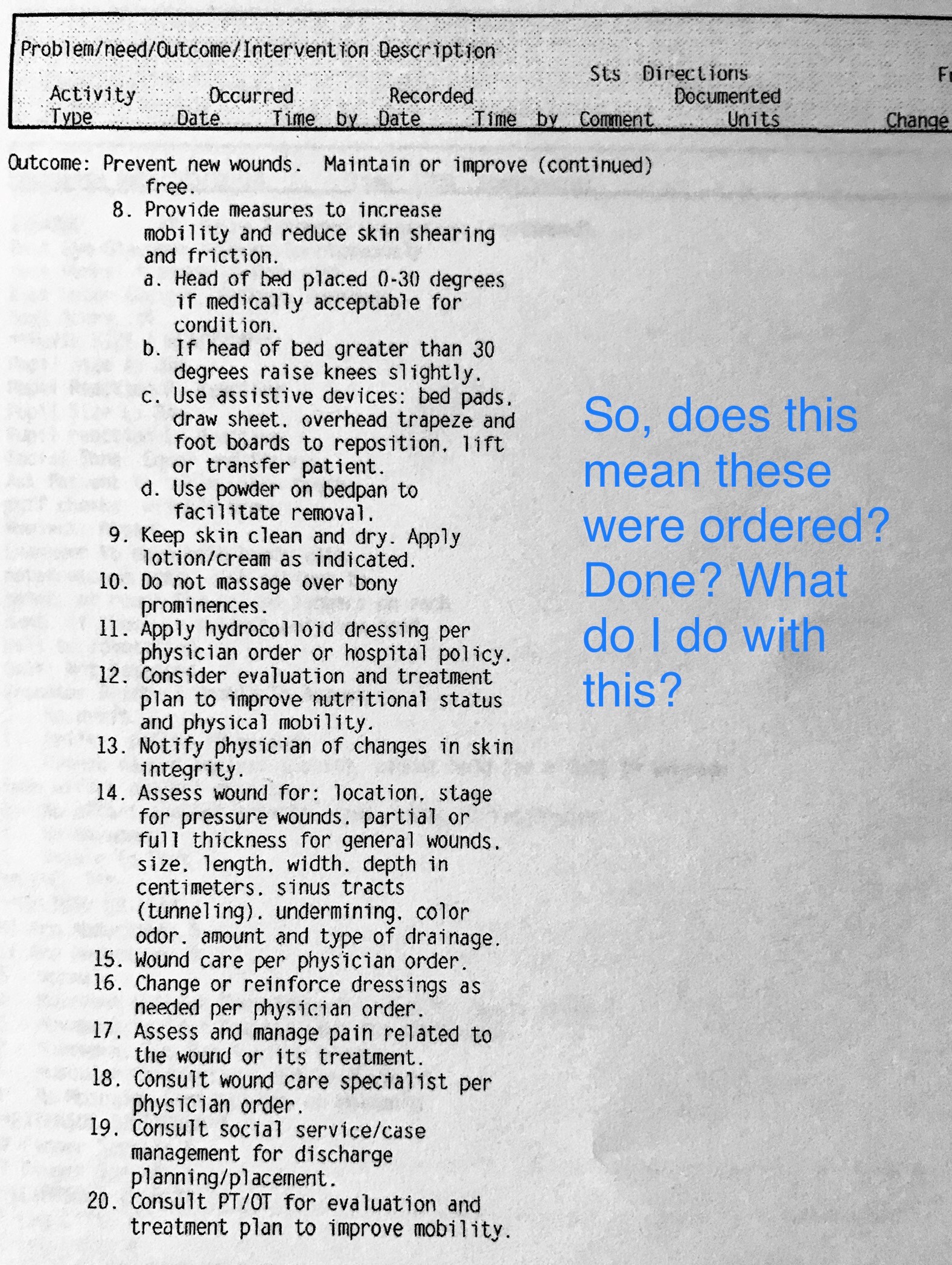
The challenge is made more difficult by the fact that the documents generated by the electronic health record (EHR) can look vastly different from the screens in which the clinical information is generated. I see this a lot with hospital EHRs when the documents are printed. It may not possible to tell which wound is which, or what dressing was put on which wound. The procedure notes do not have all the verbiage that the LCD requires to justify a treatment (because no one put that into the template in the first place). Worse, the hospital EHRs often put in pages and pages of fluff that’s not helpful or relevant (like repeated explanations of the Braden assessment or the staging system). Sometimes it’s nearly impossible to tell what got entered by a staff member. In one record I reviewed, the nurses had figured this problem out and always entered their notes in all capitals so that it was possible to tell what was typed and what was automatically generated by simply rolling forward a previous assessment. That’s not just an audit problem, that’s a medicolegal nightmare.
If you haven’t printed out a note from your EHR recently and actually read the document, you need to. Start by printing out the paper copy of the wound care encounter and with that paper copy in hand, read Donna Cartwright’s article in Today’s Wound Clinic, “How Does Your Electronic Record Measure Up Under Audit?” Go through her check list and see how your record measures up.
Also, check out Kathleen Schaum’s Business Briefs in the same issue of TWC, “Do You Have a Compliant Electronic Health Record Documentation and Signature Process?” which I mentioned in a previous blog.
These topics are so important and there is so much confusion around them that both Kathy and Donna have given me permission to post their email contact information so people can reach them directly with questions:
Kathleen Schaum: [email protected]
Donna Cartwright: [email protected]
–Caroline

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos