I recently reviewed the case of an elderly woman with a non-healing wound who had ischemic rest pain and extreme malnutrition, neither of which were addressed by the wound center at which she was treated previously. Not surprisingly she failed to improve with the application of a cellular and/or tissue based product.
Since 2014, CMS has approved the US Wound Registry (USWR) quality measure focused on arterial screening in patients with non-healing leg ulcers. The measure specifies that arterial screening be performed at the first visit. I personally use skin perfusion pressure (SPP) (in conjunction with pulse volume recording-PVR) or transcutaneous oximetry. We perform one of these studies during the initial visit of every new patient with a lower extremity wound. While Ankle Brachial Index (ABI) can help ensure ischemic patients are not put in compression (which sadly happened to this patient), it is not very useful at determining whether a wound has sufficient arterial supply to heal.
When arterial assessment of this patient demonstrated an SPP below what would be expected for healing (27 mmHg) and a dampened PVR, I immediately referred her to an endovascular expert. Because she had not had a cardiac work up, this was prioritized ahead of her leg ulcer. Fortunately she did not have serious cardiac disease. Dr. Sanjay Patel then took her to the cath lab and revascularized her. He’s provided the report below on her case. When he called me to tell me how it went, he said, “We fight PAD one leg at a time.”

- 81 year old female referred by Dr. Fife for non-healing wound on right leg with high clinical suspicious for PAD.
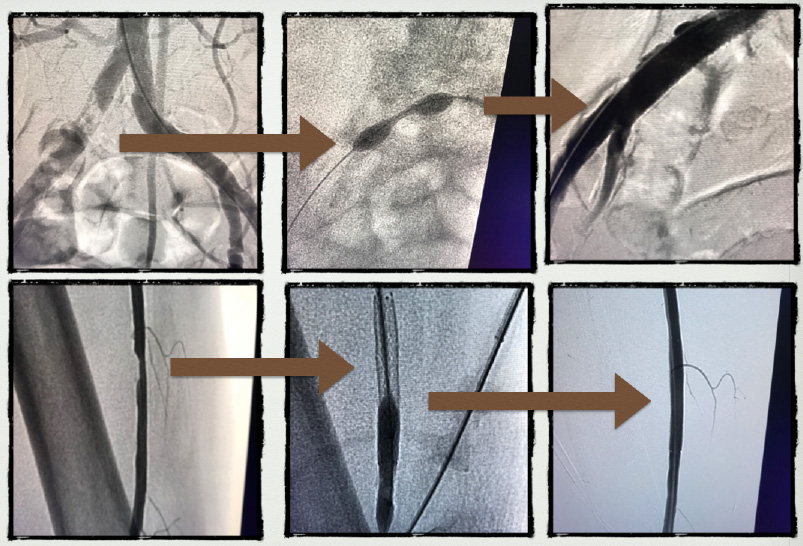
- Angiogram showed 99% Right Common Iliac lesion (70 mm hg gradient) successfully treated with 8×27 mm stent. Also treated distal Rt SFA eccentric 70% lesion with 6 x 40 mm stent percutaneously.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



Thank you for sharing, I use your articles/blogs with clinical directors and physicians. It makes them realize the importance of doing a complete work up with patients sooner than waiting to see if they improve with dressings.