I read this post by Dr. Marissa Carter with a sinking heart. Houston is now the epicenter of the second wave, and most hospitals are at capacity. The shutdown came for us before most of the population had been exposed (unlike New York City, for example), so we knew this would happen. I see no alternative than to grit our teeth and get through it. If we postpone the inevitable again (and this WAS inevitable), then we do this in flu season and as the weather turns cold. Now we have the sun. We need to pray we do not have a hurricane so we don’t have to put people in shelters.
My interpretation of the article below is that our real hope lies in a good anti-viral, and that we won’t ever go back to life as we knew it. I remember air travel before 9/11. That’s gone forever, and so is the life we had before COVID-19. We will need to focus on how to reduce risk with the least impact to mental health. Isolation is both depressing and dangerous in its own way — especially if you are a people person like I am. If you were waiting for it to “be over”, then it’s time to start thinking instead about how we adjust to the new normal.
—Caroline
SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) is the etiological agent responsible for the global COVID-19 (coronavirus disease 2019) outbreak. In the past few weeks, there have been several dramatic developments in the spread of SARS-CoV2 around the world, particularly in India, Brazil, and the USA. I will discuss these developments in more detail as data become available on trends in hospitalization and mortality rates. However, it is becoming clearer, at least in the USA, that a significant proportion of those infected are young adults, and that the vast majority of infections are asymptomatic. Indeed, Robert R. Redfield, MD, Director, Centers for Disease Control and Prevention (CDC), stated that the USA may currently have 20 million cases (about 5-8% of the entire population), which would suggest that 90% of all COVID-19 cases are asymptomatic, something the WHO might need to note. Although one might think that all these asymptomatic cases in young adults is good news, it’s not. In fact, it might be very bad news.
You Could Get Infected, Again, and Again
Two studies have come out recently, the first of which showed that 10% of almost 1,500 COVID-positive patients registered undetectable antibody levels within weeks of first showing symptoms. The disappearance of antibodies suggests that immunity is transient. The Chinese authors suggest that “after SARS-CoV-2 infection, people are unlikely to produce long-lasting protective antibodies against this virus.” This study is on the MedRXiv preprint server, so we do need to wait until it’s been peer reviewed to better assess the results. In the second study, published in Nature in Medicine, researchers compared the immune responses of 37 asymptomatic but positive patients to an equal number with severe symptoms living in the Wanzhou District in China. They determined that asymptomatic individuals reacted less strongly to infection, with 40% having undetectable levels of protective antibodies 2-3 months after the infection, compared to 13% of the symptomatic patients.
At the practical level, this means that if you had an asymptomatic infection, your chances of getting another infection (if challenged with any strain of SARS-CoV2) are high over the course of one year. But that’s not the worst of it.
Antibody-Dependent Enhancement (ADE)
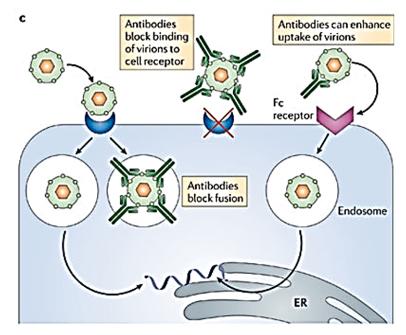
Antibody-Dependent Enhancement (ADE) is a process that occurs when antibodies facilitate viral entry into host cells and enhance viral infection in these cells (see the image to the right). Originally observed in flaviviruses (most commonly, the virus that causes Dengue fever), it has also been seen in HIV and coronaviruses. The Fc (fragment crystallizable) receptor is a protein found on the surface of certain immune cells (e.g. B lymphocytes, natural killer cells, macrophages, neutrophils, etc.). Fc receptors bind to the antibodies attached to infected cells or invading pathogens. Their activity stimulates immune cells to destroy microbes or infected cells. This means that when an individual is infected by the serotype of a particular virus (the primary infection), he or she produces neutralizing antibodies that can target the same viral serotype. However, if that person is later infected by a different serotype of the same virus (the secondary infection), then preexisting antibodies cannot fully neutralize the virus. Instead, what happens is that these sub-neutralizing or non-neutralizing antibodies first bind to the virus and then bind to the IgG Fc receptors on immune cells and mediate viral entry into these cells. In a new study, researchers reveal a novel ADE mechanism in which fully neutralizing antibodies mimic the function of viral receptor in mediating viral entry into Fc receptor-expressing cells. (In English, the second time you get infected with COVID-19, it is possible antibodies which are not able to kill the virus will instead help it enter your cells and CONTRIBUTE to infection the second time.)
Investigators have already drawn the parallel between Dengue fever and SARS-CoV-2. In particular, the authors noted: “The existence of ADE in SARS‐CoV‐2 might aggravate the COVID‐19 pandemic with higher morbidity and mortality, when convalescent patients will encounter infections in the future by possibly mutated strains.” They also said that: “ADE development should also be considered as possible adverse effects of hyperimmune globulin therapy [which is currently under study by the FDA as a possible treatment option] and vaccine development.” (In case you missed it, in English, the COVID-19 vaccine, if and when one becomes available, could make you more vulnerable to a different strain of the same virus.)
Those individuals who are infected but with very mild or asymptomatic symptoms are probably at highest risk for the ADE phenomenon. Although there were originally only two strains (L and S), that may not longer be true; there may be multiple SARS-CoV2 strains. What we don’t know is whether these strains are different enough to trigger ADE.
Parallels with the 1918 Flu Pandemic
In the 1918 H1N1 flu pandemic, one of the most interesting characteristics was the famous W-shaped mortality curve in respect of patient age in which the second peak pertained to young adults 20-40 years of age. This has been a mystery but a recent proposal by researchers has a rather alarming implication. They proposed that the major antecedent of the Spanish flu pandemic was the “Russian flu” pandemic and that the time distance between the two is crucial for understanding age-specific mortality in 1918. They argued that developing immunological memory to an antigenically dissimilar influenza subtype in early life may actually subvert the immune system, thereby increasing the risk of death when the individual is infected by a novel strain in later life. (In English, the antibodies you create to a viral infection early in life could make you more vulnerable to infection with a different virus.)
Summing Up
The really bad news is that individuals who have asymptomatic COVID-19 infections are likely to have only temporary immunity to the virus. This makes a vaccine about the only way we’re going to achieve herd immunity to COVID-19 (especially bad news given the prevalence of “anti-vaccine” individuals). Worse, a poor immune response to COVID-19 could prime the immune system to cause a much deadlier infection the second time around. In colloquial terms, this is analogous to a Trojan Horse placed in the immune system. In addition, even if we succeed in containing this pandemic, there may be consequences with regard to any future coronavirus pandemics in the years to come. (It is likely that Chinese released this virus accidentally, but next time…?)
The extent to which ADE is a problem for COVID-19 infected patients remains an unknown. Hopefully, the impact will be minor. If, however, we start seeing W- or strangely shaped mortality curves in regard to age in the next 6-12 months, then all bets are off. The long-term implications of these phenomena should cause some serious concern regarding the epidemiology of the COVID-19 disease, vaccine design, and antibody-based drug therapy.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




Dr. FIfe:
IMHO, a few comments are in order regarding your opening paragraph above.
1) This country is still in its FIRST not SECOND wave (as you stated above) as seen in the active case vs time curves published daily that have never troughed nationwide since the epidemic began in this country in mid March..
2) NY never had most of the population exposed to the virus-we just had the foresight to believe our governor and flatten the (case) curve. That is, the epidemic total case numbers over time (area under the curve=integral) were at least approximately what it would have been over a shorter time period with much larger peak case numbers without mitigation (social distancing and mask wearing.). By doing this, the state was able to keep hospital capacity manageable to date. To the best of my knowledge, our (NY) R nought is still <<1.
3) The term "epicenter" refers to above the center (as borrowed from seismology), but has been co-opted by the media to mean center.
(BTW Houston cheated our Yankees out of a World Series berth and possibly our 28th world championship in 2017-just saying)
Stay safe and stay well.
Respectfully,
Dr.Goldberg
Dr. Goldberg, you are absolutely correct in reminding us that this is still the first wave. The way things are going it might mean that we shall just see wave building upon wave so they are no longer distinct. This article (https://www.statnews.com/2020/05/01/three-potential-futures-for-covid-19/) shows graphically what that would look like.
Marissa
Drs. Carter and FIfe:
Thank you for the reference above.
IMHO, we must educate the public that flattening the case curve through mitigation (distancing, masking, and isolation) will extend a smaller continuing number of new cases over a longer period of time and help to keep hospital capacity continuously manageable, minimize deaths, and make recovered medical outcomes optimal.
I recently read a journal article that posited that the percentage of cases yielding natural viral herd immunity may be differentially less that 60-70% in different populations.
Furthermore, we must educate the public as to how important it is for the overall R nought to be < 1 (and as close to zero as possible) to relatively quickly slow viral spread (think exponential interest rate formulations, exponential mortgage rate formulations, the short story John Jones Dollar or the double the penny saved game but with the geometric factor <1.)
Finally, if we can keep the case numbers as low as possible for as long as possible, then eventually a vaccine would theoretically provide an artificial analog to herd immunity, decrease the aggregate case numbers, and would ultimately limit the otherwise unmitigated total mortality and morbidity due to this virus worldwide.
Stay safe and stay well.
Respectfully,
Dr. Goldberg