Yesterday there was a news report on one of the clinical trials using hyperbaric oxygen therapy to reduce the need for intubation in patients with severe COVID-19 pneumonia.
There is nothing magic about a hyperbaric chamber for COVID-19 related hypoxia. It is simply a very efficient method of oxygen delivery.
Normally the body is very content with breathing only 21% oxygen (with the rest mostly being Nitrogen). That’s because when the lungs are healthy, the oxygen is delivered very efficiently to the blood. The hemoglobin in the red cells grabs the oxygen diffusing from the lung air sacs and delivers it to the body tissues. In a healthy person, the percentage of hemoglobin molecules that have oxygen attached to them is >95%. That is an “oxygen saturation” of 95% or greater. This is a very efficient system.
When a patient has pneumonia, the air sacs of the lung are inflamed and it is hard for oxygen to diffuse into the blood past this barrier. As a result, the oxygen level in the blood drops, called “hypoxia.” The solution is to breathe MORE molecules of oxygen to overcome the barrier in the lung. This means breathing more than the 21% Oxygen available in room air.
There are many ways to provide supplemental oxygen, and because too much oxygen is poisonous it is not good to give more oxygen than needed. The oxygen saturation in the blood is used to guide the way additional oxygen is provided.
Hyperbaric oxygen therapy (HBOT) is one of many ways to provide extra oxygen to the blood. I have created a very simple schematic to show this. HBOT uses the physics of gas laws to dramatically increase the oxygen in the blood. Unfortunately, folks who did not take basic science in school do not understand these concepts. Oxygen is not made by a pharmaceutical company, or there would be funding for the COVID-19 clinical stuides (and I could get better graphics than the ones I created below right before my clinic started this morning).
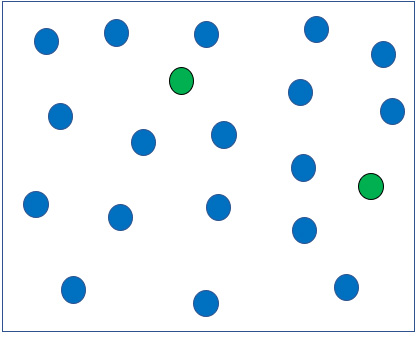
Breathing Air in a hospital room: Air is 21% Oxygen, the rest is Nitrogen. Total atmospheric pressure = 760 mmHg. Pretend there are 608 blue Nitrogen molecules and 152 green Oxygen molecules in the room.
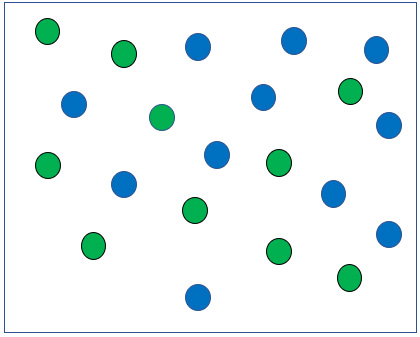
Breathing 50% oxygen in a hospital room with a face mask. Pretend there are 380 blue Nitrogen molecules and 380 green Oxygen molecules.
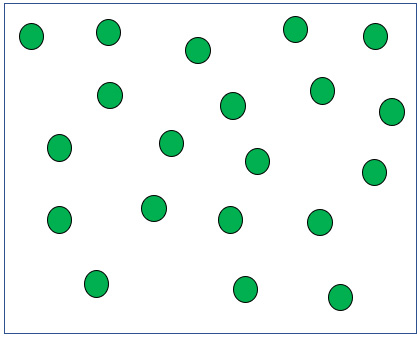
Breathing 100% Oxygen in a hospital room with a face mask. Pretend there are actually 760 green oxygen molecules.
Breathing 100% Oxygen in a helmet. Actually, I am not sure what the total number of Oxygen molecules would be, but the idea is that you can get more than 760 Oxygen molecules in a helmet.
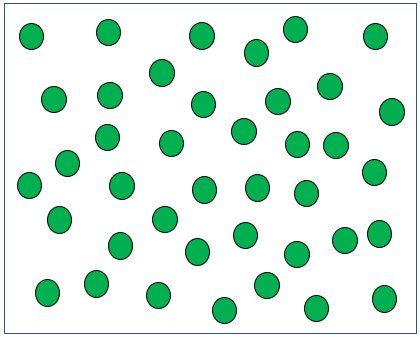
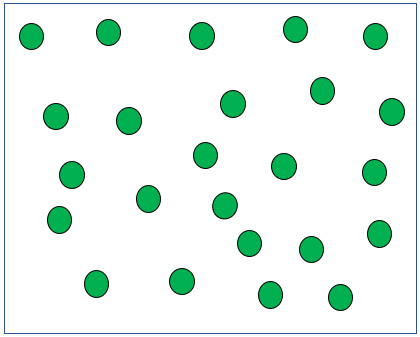
Breathing 100% Oxygen in a hyperbaric chamber pressurized to 2 times atmospheric pressure. Pretend there are actually 1,520 Oxygen molecules.
There are a lot of treatments being tried for COVID-19 pneumonia, many of which have promise, although we won’t have enough data for months (or even years) to determine which ones really make a difference. Most potential COVID-19 treatments are drugs, but I’ve even read about the use of lung radiation!
What many of those treatments do have – giving them an advantage over hyperbaric oxygen and other non-drug therapies – is funding from pharmaceutical companies that stand to make a fortune off drugs or vaccines that end up working. I am GLAD that drug companies fund this research and grateful for the drugs they develop or expand the use of – but there’s no source of funding to evaluate treatments that are NOT made by a pharmaceutical company – like Oxygen.
That’s the eternal criticism of HBOT – that good clinical trial data are lacking to support it, but exactly WHERE would the money come from to study the use of oxygen? And what is a more logical treatment for hypoxia than OXYGEN?

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




It’s just OXYGEN! And hypoxia stalks the ICUs. Hyperbaric Oxygenation can be a force multiplier in helping to stop and reverse the effects of the coronavirus pandemic.
Evidence from here in the US as well as in France, China, Israel, Philippines, South Korea, Holland, and Italy continues to show that COVID-19 patients become oxygen-starved, and that Hyperbaric Oxygenation restores oxygen delivery to all parts of the body.
Among many symptoms, the primary cause of criticality leading to admissions to ICUs is hypoxemia: lack of oxygen to body systems. Initial efforts to stem the hypoxia involved putting critical patients on ventilators. Sadly, data continue to show that ventilator patients have a greater than 50% chance of dying once they are intubated. Clearly, another less invasive and more effective way to get oxygen to body systems had to be found. Hyperbaric Oxygen Therapy (HBOT) answers the call. It is the fastest, safest and least expensive way to arrest and reverse the effects of the coronavirus.
Nassau University Medical Center and at two other sites on Long Island, are treating patients with positive indications of COVID-19. Under protocol, Hyperbaric Oxygen is arresting and helping reverse the symptoms of COVID-19. Opelousas Hospital in Louisiana has successfully treated 11 patients under a compassionate use protocol. Clinicaltrials.gov lists six trials underway or getting started, with two more in Iowa and West Virginia under compassionate use. In sum: HBOT to fight COVID-19 is already showing terrific results at reversing the effects of the pandemic and saving patients from having to go onto ventilators.
In the current pandemic the Covid-19 virus compromises pulmonary oxygen transfer leading to death from hypoxia. The FDA stated: “An increase in blood oxygen may improve oxygen delivery for vital tissue function, to help fight infection or minimize injury.” HBOT is the safest and fastest device to deliver oxygen to arrest and reverse the hypoxia brought on by COVID. It is already proved safe and effective in cases similar to COVID.
The scientific principle is straightforward against COVID symptoms: Physiological effects include diffuse, progressive lung tissue inflammation and damage, persistent progressive hypoxemia (dwindling amounts of oxygen in the body), multiple organ failure (especially liver and heart function), and inflammatory cytokine waterfall (cytokine storm). The disease has led to over 87,765 deaths in the US by May 17, 2020. HBOT infuses 20X oxygen into all body systems to overcome hypoxia due to the pulmonary distress and inflammation.
SUMMARY:
1. Right now, anyone diagnosed early with COVID is typically sent home, with the hope that they will survive the disease. More critical patients in the ER and ICU are treated with insufficient oxygen to offset incipient pulmonary distress and worse. No matter the stage of the disease, the body needs more oxygen to fight and win. The risks of conventional HBOT are low. The theoretical and actual clinical results expected are good, and the actual positive effect of HBOT use is significant. It is proven safe, harmless and likely to be beneficial when applied against hundreds of thousands of early cases of COVID-19. The treatment is less than one week and appears likely to avoid deterioration and use of ventilators when used early in the cycle.
2. HBOT is not a specific medicine, but as a good oxygen therapy method. Early intervention can be expected to reduce the incidence of severe and critical illness, thereby reducing medical care pressure, improving treatment efficiency and bed turnover rate. Properly applied, it can play a good role in the treatment of existing large numbers of patients. A growing literature of peer-reviewed science and clinical experience can be found at this site: http://www.hbot.com.
3. It is recommended to include hyperbaric oxygen therapy in the Guidelines as a means of choice for the treatment of patients infected with COVID at any stage. Given the positive data to date, it is incumbent on medical professionals to offer “informed consent” advice that includes the use of hyperbaric oxygenation as an intervention.
VIDEOS
Opelousas Hospital in engaged in compassionate use:
https://aawconline.memberclicks.net/2020-hbot-for-the-treatment-of-covid-19
https://youtu.be/7j9TJkpxyPY Dr Paul Harch: HBOT COVID-19 Protocol
Latest Research: https://www.ncbi.nlm.nih.gov/pubmed/32412891
Thibodeaux K, Speyrer M, Raza A, Yaakov R, Serena TE. Hyperbaric oxygen therapy in preventing mechanical ventilation in COVID-19 patients: a retrospective case series. J Wound Care. 2020 May 1;29(Sup5a):S4-S8. doi: 10.12968/jowc.2020.29.Sup5a.S4.
https://hbot.com/hyperbaric-oxygen-for-covid-19-report/
https://hbot.com/hbot-for-covid-19-pneumonia-and-respiratory-failure/
https://hbot.com/dr-paul-g-harch-seeks-to-examine-the-effectiveness-of-hyperbaric-treatment-on-covid-19-symptoms/
And this video: https://local12.com/news/investigates/new-treatment-promises-hope-during-pandemic-cincinnati-duane-pohlman-coronavirus-covid
Many have been calling for the HBOT replacement of ventilation ever since the beginning of the COVID 19 outbreak. The outstanding benefits of HBOT for treatment of severe Covid 19 have been known of since a few weeks after the initial outbreak in Wuhan.
Yet, our national and international medical systems have dragged their feet on recognizing HBOT, thus resulting in the unnecessary deaths of tens of thousands.
This is clearly reminiscent of Dr. Ignaz Semmelweiss, a surgeon in Hungary, who in 1851 discovered the importance of doctors applying simple hand washing before birthing newborns to save the lives of mothers who were dying in droves of puerperal fever due to the lack of hygiene by doctors. Semmelweiss wrote a book about it and gave endless lectures, yet for years, he was ridiculed, and 14 years later was eventually committed to an insane asylum (by the leading surgeon and personalities of the Hungarian medical authorities, no less) where Semmelweiss died but two weeks later at age 47.