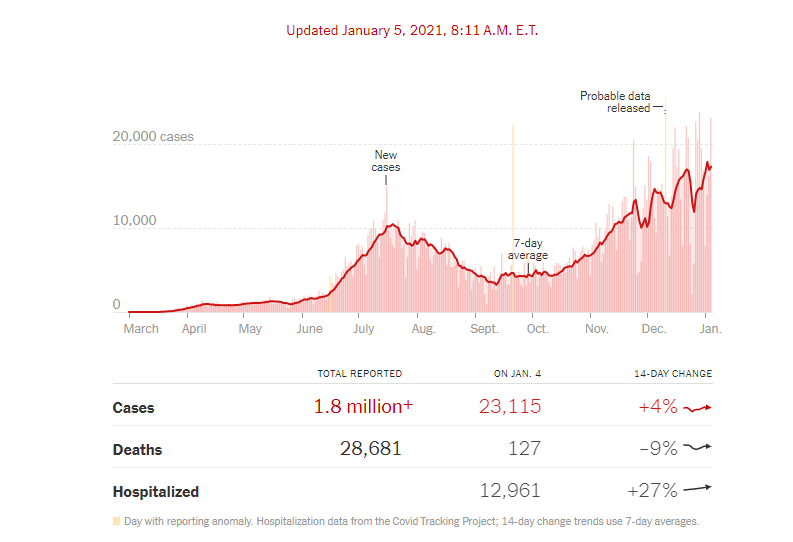
In the wake of Thanksgiving, Christmas and New Year’s, COVID-19 cases are soaring most places. Texas is not unique (see graph above). In October and early November things were looking a little better and now they are bad again. I work in a hospital-based outpatient clinic, which means that the hospital dictates our policies. They provide the space and employ the staff, so it is their party. At the beginning of the pandemic, against some criticism, the hospital agreed that wound management services were critical and did not succumb to pressure to close the outpatient wound center. To stay open, we had to agree to rigid protocols, which included not allowing family members or caregivers into the room unless there were very special circumstances (e.g. the patient can’t move themselves or is demented). I have already commented on the fact not having caregivers in the room is bad for patient care. I still need to coordinate with families and caregivers, but now I have to do it after the visit which is twice the work for me, not to mention the fact that caregivers can’t watch the dressing change process. We do what we can with family members at the request of the patient (e.g. Facetime video and having them on the phone in the room), but it’s not the same. When the pandemic numbers improved in our area, the hospital relaxed the policy about caregivers in the room, but now it’s back in force.
Yesterday a patient I am very fond of, who drives a long way and had a limb-threatening lesion originally, was so angry about the new restrictions he said he would never come back. My explanation that the hospital operates the clinic, that I don’t make the rules, or that if we did not agree to abide by them we would be closed, all fell on deaf ears. His son was furious, too. I am not sure they heard the important clinical information I was trying to convey, because they were so busy being angry about the policy.
I hate it all: wearing a mask continuously, seeing half the patients I need to see, arguing with family members over restrictions, and having my time sucked up by meetings about whatever policy is being put in place today (no, doctors cannot come in the back door and get their temperature taken, they need to stand in line with the patients at the front door…). Do these sometimes-ridiculous processes actually help reduce the spread of COVID-19? I don’t know. More than half of COVID-19 cases are spread by asymptomatic people, so taking everyone’s temperature is probably silly. I am not sure we have found anyone with a fever since we started doing this. The data are conflicting with regard to masks (at least I haven’t had a cold since last spring.) Regardless of whether these policies are helpful, I am the messenger. I don’t make the policies. I know that sounds like a cop-out, but given the choice between inefficient patient care and NO patient care, working in a hospital clinic, I chose the former.
I am praying for the success of the vaccine and that everyone who is eligible will take it. In the meantime, don’t shoot the messenger. And please do not yell at my receptionist, who is going an amazing job under difficult circumstances. We are all doing the best we can.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



Great article Dr. Fife. As a former patient of yours and someone who works for a company that manufactures wound care dressings, I can’t imagine the difficulty of providing the type of care you and your team are providing under that challenging circumstances. Continue to be the voice of reason, logic and common sense, we need more people like you. 🙂