We don’t talk enough about the relationship between sleep apnea and lower extremity edema. A lot of patients fall asleep while I am talking to them, and I don’t think the problem is my personality. Edema is THE most common diagnosis we see in the outpatient wound center (nearly every patient with any type of lower extremity wound/ulcer has edema, have you noticed that?). There are a lot of reasons for leg edema. Venous insufficiency is only one of them, and maybe not the most important one.
The patients are often chair sleepers, sometimes due to rest pain from arterial disease but often due to sleep apnea. And while I do find a lot of right heart failure that gets missed even by cardiology, many time their right heart still looks OK on echo. Still, the triad of chair sleeping, inadequately treated (or untreated) sleep apnea and leg edema is pervasive, and often overlooked.
The most useful question that I ask these patients is, “Do you sleep in the bed or a chair?” And if they say the chair, the next question is, “Why?”
Seriously, the fix for a patient like this is not venous ablation, and typical compression bandaging is not going to manage edema that extends to the buttocks. It’s hard to know where to start sometimes. All I know is that the problems I treat are all SYMPTOMS of disease.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.


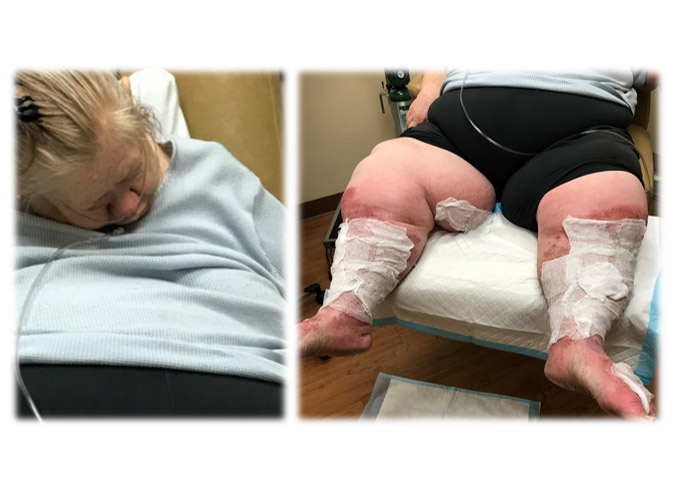

I also find a skin phenomenon known among most wound specialist as “recliner butt” Where the repetitive sleeping in the chair causes chronic tissue injury that appears deep red to purple in color. There are pictures of this in articles in the WOCN journal magazine and Advances in Wound and Skin journal.
Myra, I absolutely agree.
I would also wager that this person has incontinence issues.
Question: does greater swelling on the right foot and leg indicate anything? Perry Self
Yes, usually a sign of a blood clot
I am not a chair sleeper but do suffer from a chronic ulcer and have long term OSA. I don’t have venous insufficiency as ruled out by arterial and vein scans, am not diabetic but have had a leg ulcer for over a year now. It began to show signs of healing thanks to an infectious disease specialist who found colonization of staph (which was found before but ill-treated with oral antibiotics) and taken care of with antibiotics via a midline. Compression was finally tolerated (severe pain prevented it, even on Oxycodone) After three weeks of being painkiller free, new areas next to the old wound began to open up and the doctors are even more perplexed.
I sleep sitting upright on my couch almost every night. If I try to go to sleep in my bed I feel like there someone standing above me pushing down on my chest making it hard to breath. And if I do happen to fall asleep I end up waking up almost choking gasping for air. My feet, ankles and lower legs swell up bad. But if I elevate them higher than my heart like everyone suggests to do they swell up even worse.