Wounds are a symptom of disease, and usually the first disease we have to rule out in patients with lower extremity wounds is poor perfusion. Arterial disease is the most common reason, but not the only one. I rely on skin perfusion pressure (SPP) to determine whether the perfusion specifically to the area of the wound is adequate. I am going to post a series of articles explaining why I must have this machine or I can’t provide adequate care.
–Caroline
Because Arterial Doppler just isn’t good enough
This is an 80-year-old woman and at the time the picture above was taken, she’d had a nonhealing right anterior shin ulcer for 4 months. It began as a scratch, and clinically it’s suspicious for pyoderma gangrenosum (which is what she turned out to have). However, she’s also got ischemic rest pain. It hurts to elevate her leg, and she’s sleeping in a chair due to leg pain. PG is definitely painful, but it doesn’t cause rest pain. To make matters worse, she was placed in an Unna’s boot for her edema (caused in part by chair sleeping) and compression caused excruciating pain. Two cardiologists referred her for venous ablation because her arterial Dopplers suggested she did not have significant arterial disease.
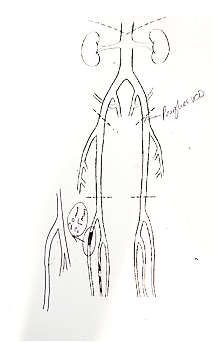
On her first visit, I performed arterial screening with skin perfusion pressure and the SPP on the right foot was only 33 mmHg with a dampened pulse volume recording (PVR). In comparison, the SPP on the left was 95 mmHg with a normal PVR. That’s a very big difference between the left and the right legs, and an SPP around 30 suggests significant arterial disease. I referred her to Dr. David Kuten, who found a nearly 100% occlusion of her anterior tibial artery, which he was able to open.
We are still struggling with her pyoderma, but at least now she can be safely treated with compression. (And folks, this is not what a venous ulcer looks like, even if she does have venous insufficiency.)
What do we learn from this?
- Arterial Dopplers are not a good way to find isolated below the knee disease.
- Listen to the patient’s history
- Just because a patient has venous insufficiency does not mean their ulcer is venous
- SPP is superior to Arterial Doppler to assess the perfusion of a wound
I need SPP to do my job. Stay tuned for more
–Caroline

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




Yep, no question!
The upper right corner has the “purple overhanging cliffs” that are classic for acute Pyoderma, although not seen that often.
…Only if you want to try to cost effectively heal the wound; eg do your job correctly. Many local vascular docs just keep intervening to try to get a trickle of perfusion through vessels with no evidence based measure of success. Then chop off a little more limb if infection evolves.
Pedal acceleration time is rolling at as a novel and practical bedside clinically relevant measure that the intervention boosted perfusion to heal the foot and limb. Look up Jill Sommerset on LinkedIn.
What’s your go-to for SPP? Used to have SensiLase, but not around anymore…
I haven’t heard this. Perimed is still in business, perimed-instruments.com
This is all a simple lesson in electrical (and fluid) flow dynamics. With SPP we are basically measuring the impedance (aka resistance or opposition a circuit presents when voltage is applied) of the stuff between the input energy or pressure head (ie the heart) and the energy sink (ie the skin/wound). Using ultrasound only evaluates the circuit’s macro anatomy and gives us no real information about the circuit’s impedance beyond the major blood vessels. Small vessel microvascular disease and extra vascular fibrosis impedes the flow of blood (voltage) and delivery of oxygen (electrons), respectively, that conventional ultrasound cannot detail, but SPP does this very nicely for us. TcPO2 further evaluates the absolute number electrons (ie oxygen) left over once hemoglobin (and plasma) is delivered to the wound through this the impeded system.
Spot on. Perfusion assessment is too often way down on the list of differentials.
I have an active PG case in a 70 year old female, with this same story, we established arterial perfusion but are now struggling to convince her dermatologist its PG because the initial biopsies only show a “nonspecific neutraphilic infiltrate” and cultures that show heavy Staph and Strep as a red herring. The wound looks exactly like the one shown above! Two doctors including myself clinically made the diagnosis of PG prior to the biopsy. I’m treating with EDTA collagen to shut off MMP pathways, hypochlorus acid to disrupt the EPS and topical gentamicin for her critical colonization. Also put her on oral doxycycline indefinitely and a short course of Augmentin mostly to “treat the conversations”.
Her wound is stabilized now but prior to initiating was expanding right before our eyes from the sterile supprative necrosis, classic PG!
She has pain with the wound of course and cannot tolerate compression which was the first treatment started when she developed her wound in the setting of illeo-occlusive venous disease. Both systems are optimized now but this saga has gone on way too long, 7 months before she came to me. Will be starting either TNF inhibitor and or ILK injections.