Wounds are a symptom of disease, and usually the first disease we have to rule out in patients with lower extremity wounds is poor perfusion. Arterial disease is the most common reason, but not the only one. I rely on skin perfusion pressure (SPP) to determine whether the perfusion specifically to the area of the wound is adequate. I am going to post a series of articles explaining why I must have this machine or I can’t provide adequate care.
–Caroline
Because arterial Dopplers aren’t good enough…
This active man in his 90’s developed ulcers on his right leg six months before this photo was taken. His dermatologist had biopsied the ulcer thinking it might be cancer (it wasn’t), and he’d been seen by his cardiologist who performed an arterial Doppler which was interpreted as normal. Because of his edema, someone wrapped his leg in an ACE bandage, and new ulcers formed on his leg.
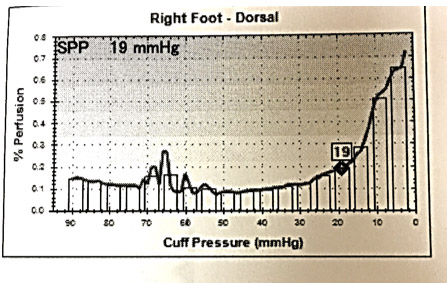
On his first visit to the CHI St. Luke’s Wound Clinic in The Woodlands, I checked a skin perfusion pressure (SPP) and the value on the right foot was only 19 mmHg with a dampened pulse volume recording. This indicates he has significant arterial disease on his right leg (any value less than 30 is BAD). I check an SPP at the FIRST VISIT on every patient with a lower extremity wound or ulcer. That’s a CMS recognized quality measure for wound care.
I did NOT put him in compression since he clearly had arterial disease. Instead, I referred him urgently to Dr. Oscar Rosales (Houston Cardiovascular Associates) who performed an endovascular revascularization. The patient healed over several months with gentle compression bandages.

What do we learn from this?
- Arterial Dopplers are not adequate for assessing the perfusion of lower extremity wounds
- SPP (combined with PVR) reliably predicts patients who need revascularization
- I can’t be a wound care doctor without my SPP and apparently neither can anyone else.
–Caroline

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




Great series of cases about the importance of SPP, thank you for posting them.