I will probably get a lot of unhappy messages about this post, but given the sweeping changes that the Centers for Medicare and Medicaid Services (CMS) has proposed for cellular and/or tissue-based products (CTPs), it might be time to “say the quiet part out loud.” The use of CTPs has increased eight fold (based on Medicare claims) in a short period of time and this equates to billions of additional dollars being spent on them. Most of that increased use is in the private physician office and not the hospital based wound center because the payment for CTPs is more favorable in the private office. CMS assumes that this massive increase in spending represents overuse or improper use — and despite all the hand wringing, we have no way to prove otherwise. The tools CMS has at its disposal are blunt. All they can do is reduce payment knowing that a reduction in usage will follow.
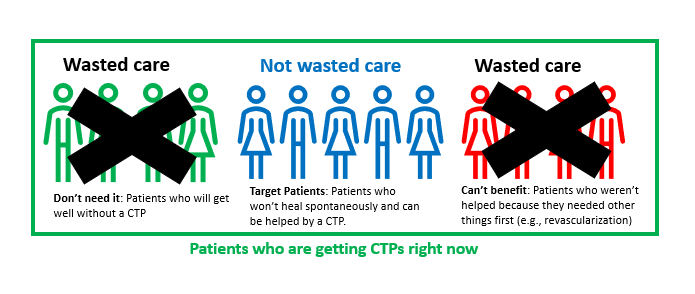
While most of us want to do the right thing for patients and believe we are doing the right thing, it’s fair to assume that not every physician using CTPs is motivated by altruism. I am going to assume that the current use of CTPs represents at least 3 types of wounds/patients: 1) those who don’t need a CTP or advanced therapeutic (AT) because they are going to get well anyway, 2) the target population of patients who will NOT heal spontaneously but who can benefit from an AT (because they have adequate arterial supply and good nutrition, for example), and 3) the patients who can’t benefit because their wounds are too severe or they haven’t had the necessary basic care. I have no idea what percentage of current CTP use falls into each of these 3 categories. I would be happy to get your thoughts on what percent of CTP patients fall into each of these categories.
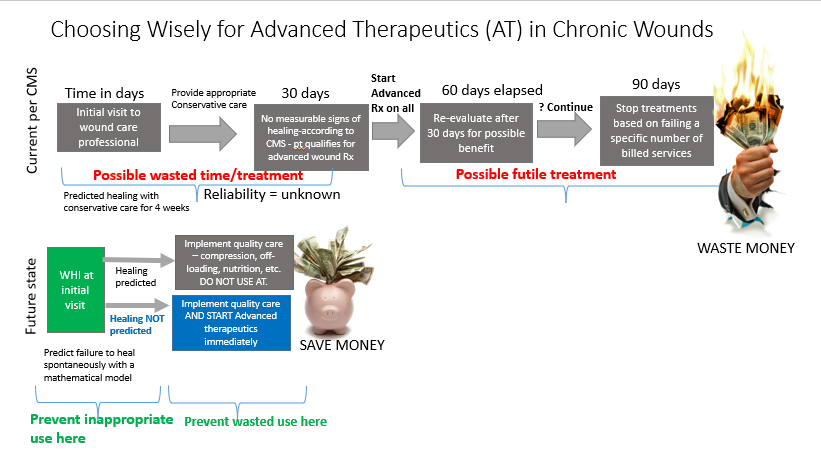
CMS has few options other than the Nancy Regan “just say no” approach to overuse. They can’t stop wasted care without limiting access to necessary care. Many years ago, I published a paper in Plastic and Reconstructive Surgery explaining the way that predictive models could be used to better allocate hyperbaric oxygen therapy (HBOT) in diabetic foot ulcers. There was exactly zero interest in this concept for obvious reasons. Making effort to find the patients who need any therapy means NOT providing therapy to the patients who do not need it. Reducing use of any AT reduces revenue. However, if the alternative to finding the RIGHT patients for an advanced therapeutic is that no patients will have access to it – maybe it’s time to talk about how we can choose wisely for CTPs.
I know how we could fix the problem of improper use of CTPs, but I also know that no one wants to do it. We would have to identify the patients who really need them and not treat the ones that don’t need them. And, we’d have to “do the right thing” with regard to meeting the standard of care. We can do both. We have accurate predictive models to do the first, and we could use quality measures to do the latter – but no one wants to do that. It’s a lot of work for the practitioner to “choose wisely,” and a totally lost cause if they get paid the same as the doctors who aren’t adhering to best practices. I do not see manufacturers supporting these ideas or clinicians being willing to implement them.
There will be a lot of whining about how vulnerable patients will get hurt by CMS proposed policy on CTPs – but no discussion about limiting the wasted use that caused CMS to act.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



Dr. Fife – I am in total agreement with you. I appreciate your knowledge and years of expertise. I’ve read the proposed rule and your blog, but I can’t seem to determine which skin substitute codes the packaging in the physician office will impact. Are you able to share the series of codes this change will potentially impact? Is it the 10 A codes that were developed last year or a different set of codes? Thank you so much for your response! Bria