
I have seen a lot of drug induced ulcerations and I bet you have, too. Some of them can be horrific. A colleague just emailed me to ask if I’d seen any Xylazine-related ulcerations. Xylazine (a veterinary anesthetic) can be used to cut fentanyl, heroin and sometimes methamphetamine. I don’t know the mechanism by which it causes ulceration, but I’ve included some photos below to illustrate the difference between wounds caused by a vascular injection (even an accidental one) and a subcutaneous injection of a variety of drugs.
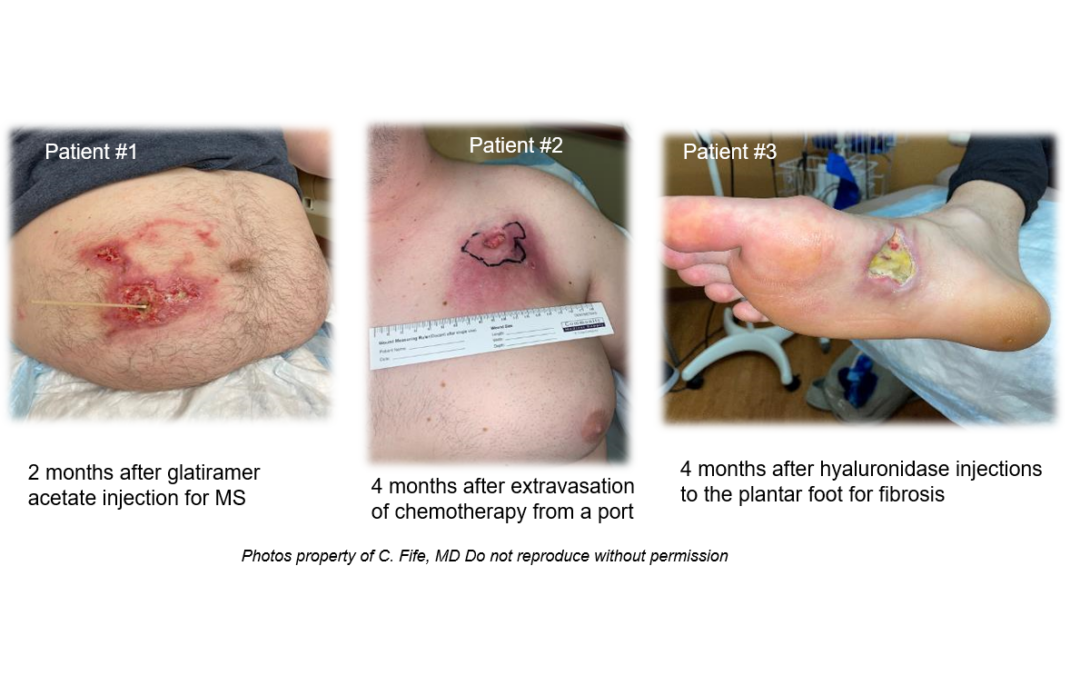
Patient #1 has multiple sclerosis and was self injecting glatiramer – supposedly subcutaneously. However, you can tell that there was an inadvertent injection into a superficial vein based on the pattern of the tissue necrosis and inflammatory reaction. In contrast, Patient #2 had extensive fat necrosis around his chemotherapy port. There was a very large area of necrotic fat – so large that it required a plastic surgical excision and closure. Patient #3 underwent an intentional subcutaneous injection by a physician with hyaluronidase, used off-label for plantar fibrosis. Patient #4 underwent injection with a sclerosing agent for varicose veins and ultimately required surgical debridement.
I’ve seen ischemia and necrosis of areas of the face after aesthetic injections (usually accidentally into a vein). The mechanism might be direct toxicity to the tissue or in the case of vascular injection, ischemia from reduced venous return or arterial supply. Once it’s happened, it may be impossible to stop the cascade of events. Hyperbaric oxygen therapy has been helpful anecdotally for patients with ischemic tissue after a cosmetic injection –but time is of the essence for HBOT. I think it’s time to start talking about drug related ulcerations – whether they are caused by prescription or recreational drugs and regardless of whether the drug was injected by the patient or the physician. I have submitted at least one report on the FDA’s website but I have no idea if anyone pays attention to that.
I am curious about your experience. Let me know what you are seeing.
Also, check out this article from Texas Medicine Today: Feds Declare Xylazine an Emerging National Threat in Opioid Crisis

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



I have not seen any that I thought to be a specific relationship. Just the ongoing long med lists of chemicals that debilitate mitochondrial function. Regarding the venous ablation case, they appear to have significant livedoid vasculitis (LV) which can get quite angry and is quite challenging. Although I have seen ablations in these people, I don’t recall seeing one when the inflammation was high or on the upswing. Regional cytokines and cellular iron dumping in the area could leave to a perfect storm of oxidative stress. Just thoughts. PS I’ll take any wizardry you can offer when treating LV. i have never failed to heal one, but their has to be a better/shorter way.