Dr. Fife,
I wanted to illustrate how an office-based doctor using Cellular Tissue Products / Skin Substitutes is often unable to cover the cost of this treatment – if they follow the Medicare rules. At the very least, in many cases, I wanted to illustrate why an office-based practitioner is dependent on collecting the secondary insurance payment or the patient-responsible portion – if they are to make ends meet.
Here’s an example of a redacted invoice. I won’t point out the name of this product although most readers might be able to figure it out. The problem is NOT with the brand or the product itself. I am simply using this product as an example of why “following the rules” – which our practice does – can mean losing money with CTPs.
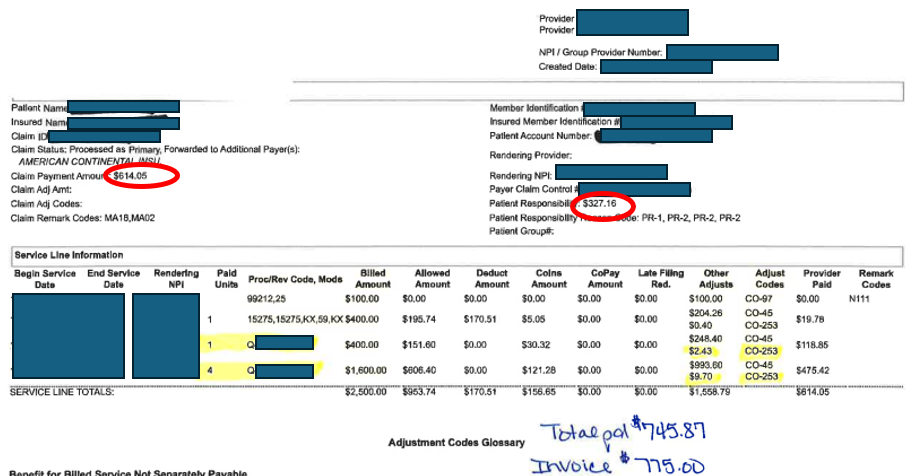
In the case of this product, the invoice price is $775 (meaning, that’s what I actually paid for the product). The “allowable” amount that Medicare can reimburse me for the product is based on the published Average Sales Price (ASP). The ASP for this product is $758, and that means that Medicare pays $606.40. As everyone understands, I must get the remaining 20% ($151.60) by billing the patient’s secondary insurance, or from the patient themselves if they do not have a secondary insurance.
Please note that the ASP ($758) is $17 less than the list price ($775). In other words, even if I collect the full amount of the Medicare allowable, I lose money!
But that’s not the whole story. It’s worse than that. There’s a 2% “sequester” in place. This means that I get paid 2% less by Medicare for EVERYTHING. Thus, what Medicare will actually pay me is not $606.40 but $594.27 after the sequester. The secondary should still pay $151.60, but the total is now only $745.87. Thus, I will lose $29.13 on the application of the product after the sequester– assuming that I am able to collect the copay. If I am not able to collect the copay, then I will lose $151.60 on each application of this product plus the sequester reduction of $12.13 for a total loss of $163.73 per application. This is unsustainable. It is simply not possible to “make up” that loss using the application fee. If one uses the manufacturer’s recommended number of applications, let us say 10, then you are now out of pocket a total of $1,637.30 for each “episode of care.”
Now let’s consider Medicare’s new requirement that I must use products that are almost exactly the size of the ulcer. This size requirement makes it increasingly difficult to use CTPs appropriately, since the smaller sizes are more expensive per sq cm! Unfortunately, the ASP pricing assumes uniform pricing per square centimeter regardless of the actual invoice price. Thus, when smaller pieces are used, the loss per application is even greater. However, I can’t use a larger piece (the price of which is closer to the ASP) because the charges will be denied for unnecessary wastage. It is truly a Catch-22. Until Medicare places a sliding scale of “average” pricing based on the actual cost of the product per sq cm, patients will not be getting the current standard of care because physicians cannot afford to subsidize patient care.
I cannot charge more than Medicare allows, yet the Medicare allowable does not cover the basic cost of the product.
The loss of revenue inherent in using CTPs raises many ethical issues. For doctors who play by the rules, it means that CTPs can be offered only to patients with secondary insurance or to those patients who are wealthy enough to afford the copay. Keep in mind that the more expensive the CTP is, the higher the copay – which is a major reason not to use products that are, for example, $3,000 per cm2, when a product that is a fraction of that price works just as well.
I do not condone that fraud that is occurring with the use of CTP/skin subs, but I would like to point out that the only way most clinicians can keep from losing money is by taking advantage of some “under the table” discounts on the cost of the product. Our office does not accept under the table discounts, and that is a major reason why we use CTPs only rarely. This translates directly to disparities in care.
Medicare and other insurance carriers need to be aware of the impact that their policies are having on patient care and equity. Nothing can change for the better unless all the unforeseen consequences of their policies are addressed, or until manufacturers start charging the same price per square centimeter for all product sizes. (Please stop telling me that smaller products cost more for you to make – I feel sure that for manufacturers, these issues are manageable). The bottom line is that under the table discounts would not be necessary if the pricing was within the reimbursement guidelines that have been established by Medicare and other insurance carriers.
[Name withheld]

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.