An article in JAMA Dermatology reviews the wound characteristics of a series of 29 patients hospitalized with confirmed xylazine exposure. Xylazine was originally developed as a veterinary sedative, anesthetic, and muscle relaxant. Although xylazine is not an opioid, it is a central nervous system depressant with opioidlike effects, including sedation, slowed heart rate and pupillary constriction, similar to the effects produced in people by its pharmaceutical cousin clonidine. It was first identified as an adulterant in heroin supplies in the early 2000s, but is increasingly found in illicitly manufactured fentanyl.
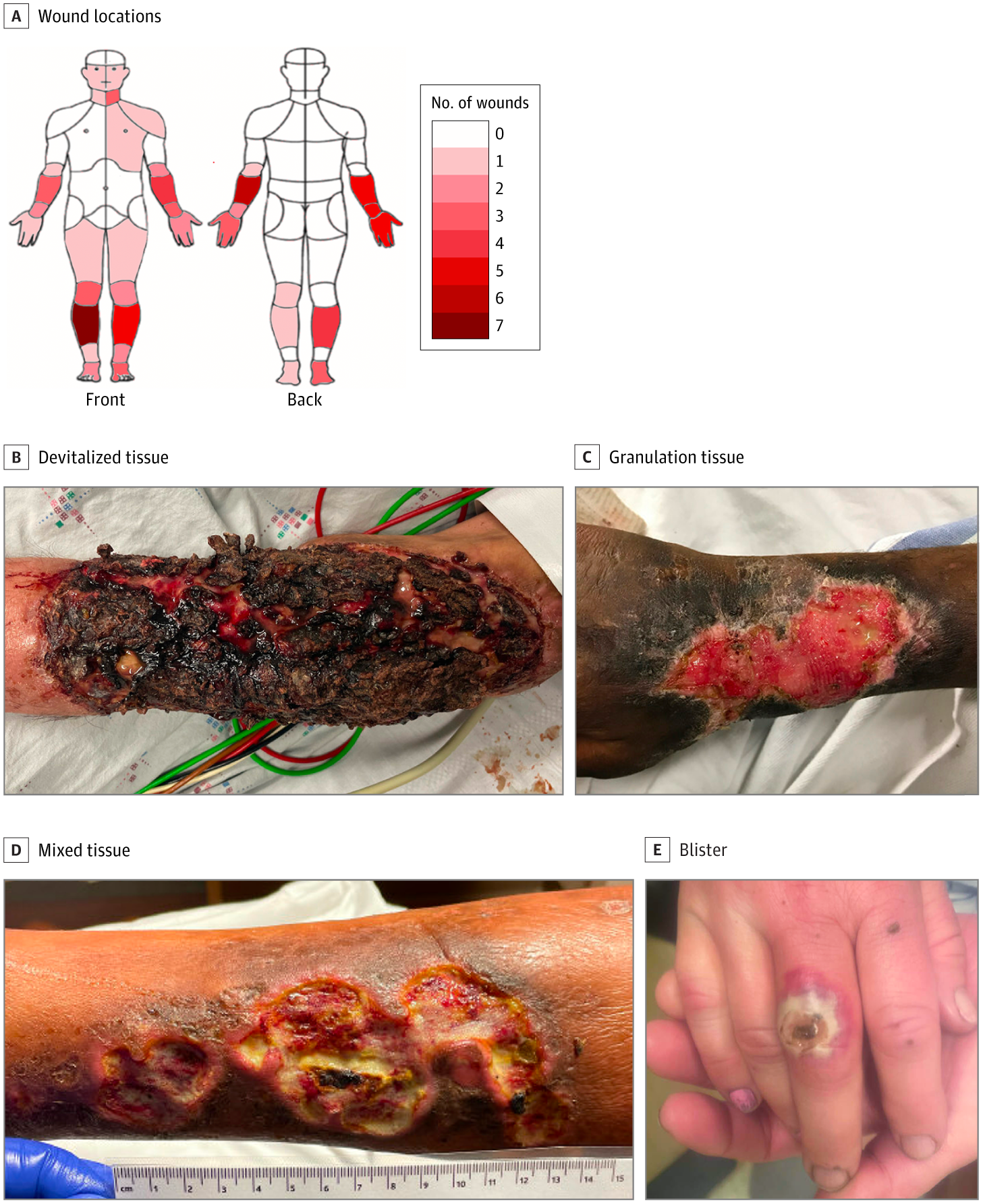
Xylazine may be responsible for an emerging pattern of necrotizing wounds. The JAMA Dermatology article reviews a case series from 3 academic medical hospitals in Philadelphia, Pennsylvania who presented with wounds and in whom xylazine detected with urine gas chromatography–mass spectroscopy. The cases are important because some previously published cases of soft tissue injury/necrosis in fentanyl users did not confirm xylazine exposure so it has not been clear whether the ulcerations were caused by the xylazine or some other adulterant. In this case series of 59 wounds among 29 hospitalized patients with confirmed xylazine exposure related to routine opioid injection, wounds were commonly located on extensor surfaces of the extremities, frequently had devitalized wound beds, and were more likely to have larger and necrotic wound beds the longer wounds had persisted. Most of the ulcers were on the extremities and some involved exposed bone or tendon. Not surprisingly, most of the wound beds involved non-viable tissue (eschar or slough). Perhaps the most important issue was not emphasized in the report, and that is 89% of the patients in the case series were younger than 50.
This remains a rare cause of non-healing wounds, but should be among the differential diagnosis for “younger” patients with deep, necrotic ulcers, particularly on the upper extremities.
Additional Reading:
This case of skull osteomyelitis from xylazine was just published in JAMA Dermatology. Skull Osteomyelitis Associated With Scalp Xylazine Injection | Dermatology | JAMA Dermatology | JAMA Network

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



