A 2022 study in JAMA Association found that the Quality Payment Program (QPP) was “approximately as effective as chance in terms of identifying high versus low quality performance.” That’s a big “oops” when you can lose up to 9% of your Medicare billing based on your “score” inside a system designed to favor (big) practices with “people” to handle the stupid stuff. Unless they are participating in an Accountable Care Organization (ACO), the primary way that most clinicians participate in the QPP is via the Merit Based Incentive Payment Program (MIPS). Since 2017 when MIPS began, the potential penalties have continued to increase (with a pause on many requirements during COVID), and monetary bonuses for a perfect score are less than the cost of participating (top bonuses are generally <2% of Medicare claims). In 2024 and for the foreseeable future, the maximum penalty associated with MIPS is a whopping 9% of Medicare payments. When added to the 3% sequester, practitioners who don’t get MIPS figured out could end up closing their doors – given the narrow margins associated with most practices these days.
Just as a reminder, the QPP program was the “good option” to fix physician payments under Medicare. The Medicare Access and CHIP Reauthorization act (MACRA) of 2015 eliminated the Sustainable Growth Rate (SGR) formula because if it had been implemented as written, that year it would have resulted in a 25% decrease in physician payment.
MIPS had good intentions behind it when it was implemented in 2017. Physicians were already starting to sink under 3 different but mandatory reporting requirements – including the requirement to adopt an electronic health record (EHR) which began around 2009. The aim of MIPS was to streamline several disparate quality-reporting programs. Instead, MIPS increased the burden of reporting. A JAMA Health Forum study found that physicians spent an average of $12,800 per practitioner and over 200 hours a year to comply with MIPS. In the 2025 final Medicare physician payment schedule, CMS itself estimated that MIPS would impose health-system burdens equating to 586,877 hours and cost more than $70 million.
The burden of MIPS unfairly impacts small and rural practices across the country which have fewer resources to divert from patient care to comply with bloated, and ever-changing MIPS requirements. The unfair impact of MIPS is evidenced by the fact that in 2024, 45% of solo practices, 31% of small practices and 18% of rural practices were penalized under MIPS, compared to 14% of practitioners overall. Even more worrisome, according to CMS’ 2022 report on the program, nearly 30% of physicians in solo practice got the maximum 9% penalty. These penalties have occurred even though there is no evidence to show that MIPS has improved even one healthcare outcome — and there is abundant evidence to show that it is decreased the quality of medical care.
The American Medical Association (AMA) has proposed a new, budget-neutral incentive payment system that every state medical society and more than 100 national specialty societies (PDF) have endorsed. It is called the Data-Driven Performance Payment System MIPS is broken and must be replaced. Here’s how. | American Medical Association. I agree with most of the AMA’s recommendations. I would like to see some “big picture” improvements rather than focusing on incremental improvements in an overly complicated system.
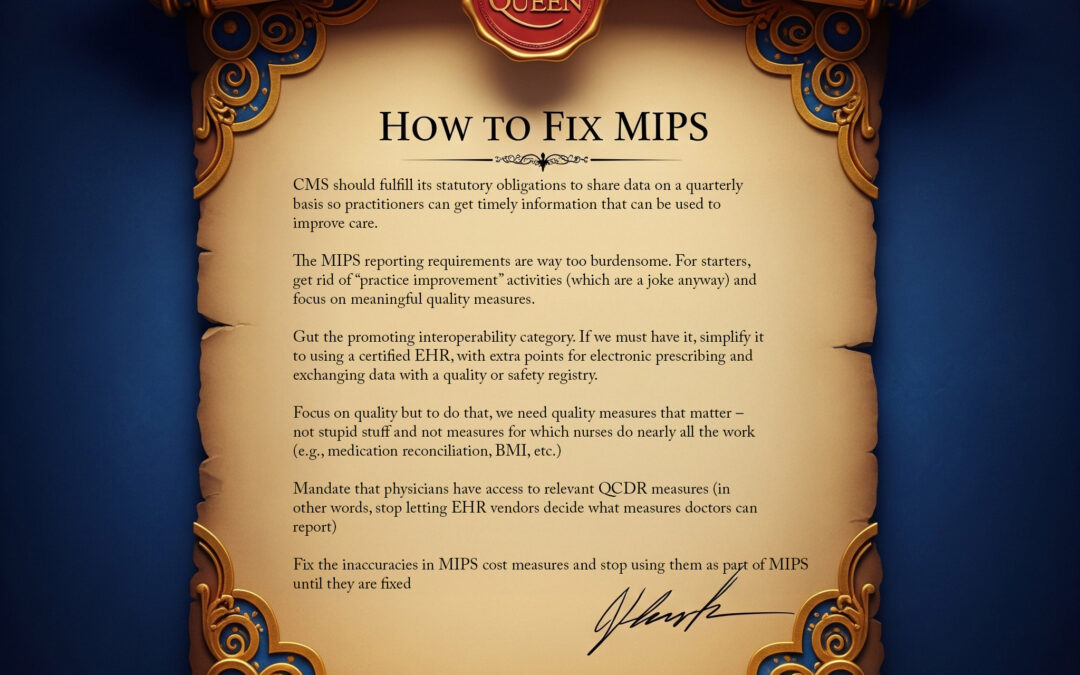
I view all of these issues through the lens of wound care, so here’s the Queen’s list of stupid stuff we should fix about MIPS (for wound care doctors):
- CMS should fulfill its statutory obligations to share data on a quarterly basis so practitioners can get timely information that can be used to improve care. (That was the POINT in the beginning)
- The MIPS reporting requirements are way too burdensome. For starters, get rid of “practice improvement” activities (which are a joke anyway) and focus on meaningful quality measures.
- Gut the promoting interoperability category. If we must have it, simplify it to using a certified EHR, with extra points for electronic prescribing and exchanging data with a quality or safety registry.
- Focus on quality but to do that, we need quality measures that matter – not stupid stuff and not measures for which nurses do nearly all the work (e.g., medication reconciliation, BMI, etc.)
- Mandate that physicians have access to relevant QCDR measures (in other words, stop letting EHR vendors decide what measures doctors can report)
- Fix the inaccuracies in MIPS cost measures and stop using them as part of MIPS until they are fixed
I am particularly concerned with the attempt to develop a “non-pressure ulcer” cost measure. Several Alliance members (including me) served on the Clinical Advisory Panel for this cost measure and were vocal in their lack of support for the final measure which would hold wound care practitioners responsible for care delivered by other practitioners after the patient had left their practice. Errors in the codes included in the measure were not addressed by the contractor (Acumen) prior to finalization of the draft measure, and the detailed concerns of experts were dismissed by Acumen (with contractors stating that the Advisory Panel just didn’t “understand”). While the Alliance supports the development of a wound-care relevant cost measure, field testing of the draft measure demonstrated critical errors. Should the cost measure be implemented, the lack of wound care relevant, national quality measures makes it impossible to develop a useful MIPS Value Pathway (MVP) relevant to chronic (non-pressure) ulcers.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



do you think MIPS could be utilized to stop the fraud in CTP use? Id be interested to compare costs for similar types of wounds receiving different treatments – one with CTP and one without. Also, what are the long term outcomes after CTP use? What if CTP reimbursement was clawed back if the patient who received these applications still lost their limb/digit/etc within 3 mos because the wound care utilized was inferior and the CTP was relied on for healing – therefore the wound healed in spite of the provider and not because of the provider. These outcomes could be tracked through MIPS and save our industry.