The White House Office of Management and Budget (OMB) spent 6 months reviewing a proposed rule to ease Medicare-participation requirements called, “Regulatory Provisions to Promote Program Efficiency, Transparency and Burden Reduction.”
CMS has promised to “reform Medicare regulations that are unnecessary, obsolete, or excessively burdensome on healthcare providers and suppliers.” Let’s forget for a moment the irony of a massive new federal regulation the purpose of which is to reduce federal regulation.
Follow me on this issue. The Obama CMS banned “step therapy” in Part B drugs. This is a process in which some drugs are approved only after a less expensive drug has been tried and has failed. The reasoning outlined by the Obama CMS in a 2012 memo was that Medicare Advantage plans could not impose barriers on drugs unless the same barriers existed in fee for service Medicare. However, CMS Administrator Seema Verma has now announced a reversal of the step therapy ban in order to help Medicare Advantage plans bargain for lower drug prices. That means “step therapy” in Part B drugs is now allowed by Medicare Advantage plans. Personally, I am not convinced it was ever OUT.

Here’s a screen capture from my EHR’s electronic prescribing module telling me I can’t prescribe Santyl because it’s a “tier 4” drug and I need to use a lower tier drug first. I wonder what that drug would be? Send me a message on LinkedIn if you know what a lower “tier” option would be that I should try and fail with before I prescribe Collagenase.
The Obama CMS also banned Medicare Advantage plans from using prior authorization as a method to limit access. Currently a bipartisan group in the House is trying to expand the Obama era ban on prior authorization using the same argument, that Medicare Advantage plans cannot erect barriers that do not exist in fee for service Medicare.
 But, here’s a screen capture from my electronic prescribing program for Becaplermin (Regranex) telling me to get prior authorization before I can use it on a diabetic foot ulcer. I received both of these messages from the same Medicare Advantage plan during the Obama years.
But, here’s a screen capture from my electronic prescribing program for Becaplermin (Regranex) telling me to get prior authorization before I can use it on a diabetic foot ulcer. I received both of these messages from the same Medicare Advantage plan during the Obama years.
However, I admit, I’m really not that worried about collagenase or platelet gel. What’s worrying me is that it’s a waste of my time to even TRY to use a cellular product on a patient with Medicare Advantage. Maybe it’s just the plans in my area, but they don’t cover any products that came to market under the 510(k) approval process (which is all but 2 of them). And, I have to call to and have a “peer to peer” to get authorization for any advanced therapeutic.
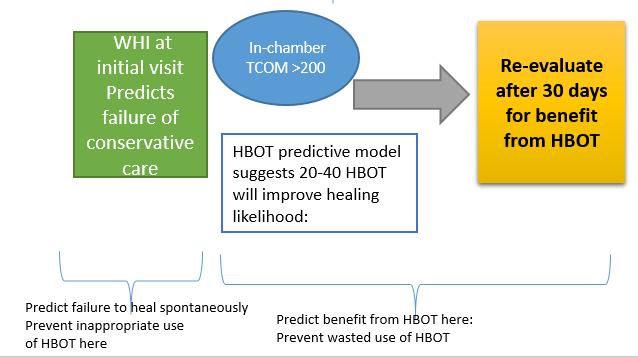
Truthfully, I can’t blame the HMO Medical Directors. We have failed to make the case that their beneficiaries will have a problem healing since they keep being told we heal 95% of their patients – or is it 75% now? Either way, it’s no wonder they aren’t worried about their beneficiaries needing advanced therapeutics. In their mind, we are just making money at their expense, raising the cost of care among patients who are all going to be just fine anyway. Because that is what we have been telling them. And so, they are quite happy to tell us “no,” through that prior authorization that isn’t supposed to happen, and the step therapy that is back to being OK. Of course, we could use the Wound Healing Index to identify which patients are statistically likely to need advanced therapeutics to heal. But that would be way too efficient and transparent.
Fife CE, Eckert KA, Carter MJ. An Update on the Appropriate Role for Hyperbaric Oxygen: Indications and Evidence. Plast Reconstr Surg. 138(3 Suppl): 107S-116S, 2016

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.