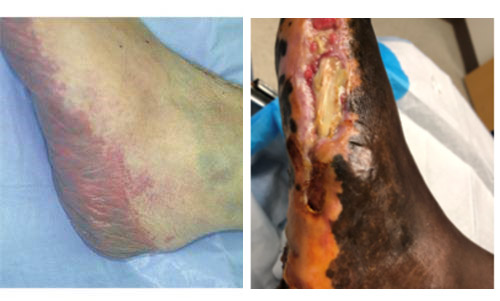
This is the left foot of a 34-year-old African American woman who spent 21 days in the intensive care unit, hypotensive from sepsis and on vasopressors with disseminated intravascular coagulopathy (DIC). She lost all the toes on her right foot from ischemic necrosis. She also developed an eschar on the plantar heel of the right foot and ischemic changes along the left lateral foot.
How did she experience pressure to the plantar surface of the foot and the lateral foot when she was supine in the ICU? The answer is, she didn’t. These are NOT pressure injuries. What happened to her left foot was due to a reduction in circulation to the medial calcaneal branch of the posterior tibial artery as a result of hypotension, vasoconstriction and/or occlusion from a clotting disorder.
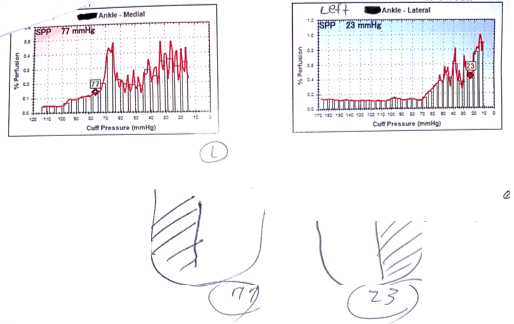
I performed a skin perfusion pressure (SPP) study to determine whether the perfusion through these vessels was adequate to support healing. The SPP of the lateral aspect of the foot was only 23 mmHg with a poor pulse volume recording (PVR) wave form. She underwent an angiogram and had no large vessel atherosclerotic disease. The pressure was low in this angiosome because of her coagulopathy and with a value lower than 30 mmHg, it is below that which is usually needed to support healing.
These were called “pressure injuries,” but like many similar foot lesions in ICU patients they are actually vascular infarctions. The reason you can tell that is that the anatomical distribution is the angiosome supplied by the medial calcaneal branch of the posterior tibial artery, depicted in the cadaver study by Dr. Chris Attinger, below. Here is a figure from Attinger’s “Vascular anatomy of the foot and ankle,” which demonstrates the angiosomal perfusion of the foot using injections of dye into cadaver specimens.

The medial calcaneal branch is the first main distal branch of the posterior tibial artery (above). Its angiosome includes the medial heel (center), the plantar heel, and the lateral plantar heel up to the lateral glabrous junction. (from Attinger C. Vascular anatomy of the foot and ankle. Oper Tech Plast Reconstr Surg 1997;4:183)
Ref:
1Angiosomes and Wound Care in the Diabetic Foot, Mark W. Clemens, MDa , Christopher E. Attinger, MDb. Foot Ankle Clin N Am 15 (2010) 439–464 doi:10.1016/j.fcl.2010.04.00

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




Did diabetes cause this?