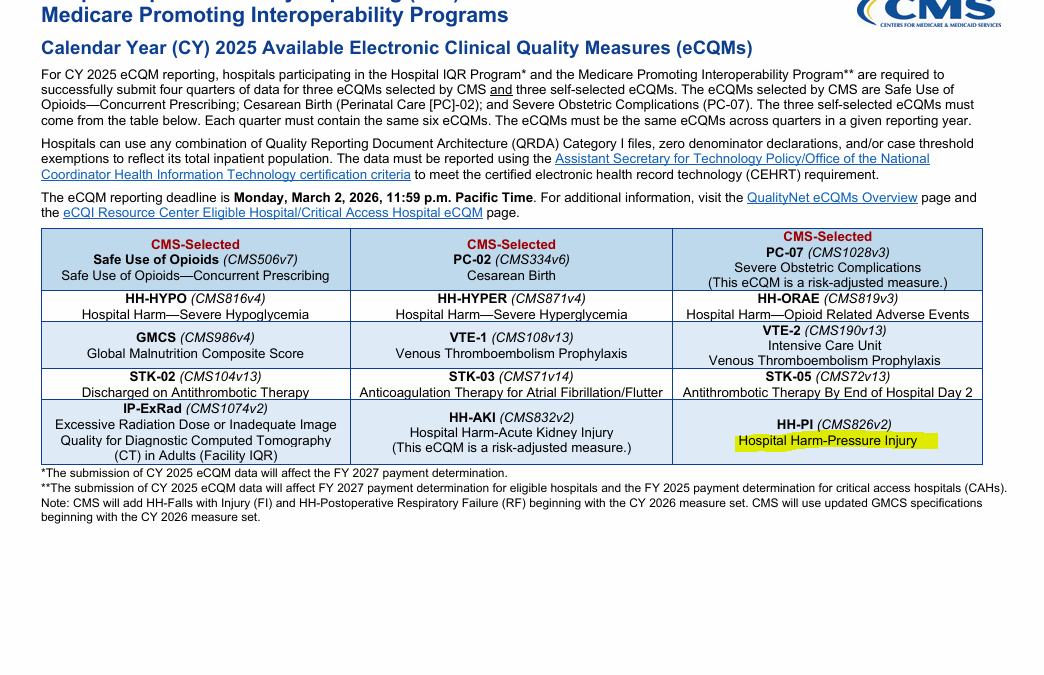
In the August 28, 2024 Final Rule (CMS‑3401‑F), CMS (the Centers for Medicare and Medicaid) updated the list of “Hospital Harms” in the Hospital Inpatient Quality Reporting (IQR) requirements. The new rule became effective this year. I will skip the explanation of the way that a hospital’s electronic health record (EHR) is supposed to have programming to facilitate the direct transmission of this information from the EHR via an eCQM (electronic clinical quality measure).
It is not new for hospitals to have to report Stage 3 and 4 pressure injuries (still called pressure ulcers in the ICD10 code book) that were “acquired” during admission. However, this Hospital HARM measure captures adult inpatients who develop a new Stage 2, 3, 4, deep‑tissue, or unstageable pressure injury while hospitalized, events which can lead to a one-fourth reduction in their annual Medicare payment update. The part that is new is the addition of Stage 2 injuries to the list of “harms” that have to be reported. I should add that in 2025, reporting Stage 2 pressure injuries is voluntary, but CMS plans to make it mandatory in 2027.
Just a few reasons why everyone has lost their minds
In 2016, the NPIAP arbitrarily changed the definition of a Stage 2 to include only partial thickness lesions. This means that a Stage 2 lesion is as severe as a superficial ruptured blister. A Stage 2 lesion still has skin on it, folks. Stage 2 lesions cannot have any slough or granulation tissue – findings that are only associated with full thickness lesions. In fact, it’s almost impossible to get an outpatient a surgical dressing for Stage 2 lesions because they are so superficial. And I have news for everyone – partial thickness lesions of this nature are ACUTE WOUNDS – they are not chronic ulcers. They don’t belong in the “ulcer” section of the ICD10 code book. When the NPIAP made this new definition, Stage 2s should have been moved to the acute wound section – with all the other acute INJURIES.
Since pressure injuries do not “progress” through the numbers (a newsflash to many people), Stage 2 lesions do not ever become Stage 3 or Stage 4 lesions. It is true that a blister can be the first sign of a more serious skin problem – but not because the problem “progresses” –but because an injury that already happened EVOLVES. Think about what happens when you burn your finger in the kitchen. A day later, you develop a blister as the evolution of the original burn and not because it is getting “worse”. There are no good data to tell us the likelihood that a partial thickness area of skin loss is a harbinger of a more serious problem vs. superficial epithelial loss from local friction. It will be nearly impossible for hospitals to implement this policy which will require them to report even the most minor area of skin disruption as a hospital HARM.
This is only one of the downstream effects of re-naming all pressure ulcers as “injuries” (a term which should have been limited to Stage 1s). However, to be fair, CMS considered them “hospital harms” long before the name was changed to something more favorable for plaintiff’s attorneys. It is also the downstream impact of the National Quality Forum (NQF) which for many years stated in their documents that pressure ulcers were ALWAYS due to a “failure of care” and classes them with patient electrocution from medical devices. By the way, CMS has never called pressure ulcers “never events.” We have the NQF to thank for that canard.
This should be the last straw for hospitals and their insurance carriers
This needs to be the last straw for hospitals. It’s time for the American Hospital Association, their insurance companies and their defense lawyers to stand up. It’s time to fix the staging system – and the answer is not calling severe pressure ulcers “skin failure,” a diagnosis that requires a forensic evaluation of the chart and which is not anatomically accurate since these tissue infarctions are not limited to the skin. The well intentioned initiative to get the concept of “skin failure” into ICD10 is not going to fix the inclusion of Stage 2 “pressure injuries” on the list of “hospital harms.” Just like severe pressure injuries, this regulatory overread formed from the “inside out.” Fixing it means throwing out the current staging system and replacing it with one that is consistent with human pathophysiology. Until enough sane people stand up to this, hospitals had better get prepared to pay monetary penalties for minor skin lesions and to deal with a lot more frivolus litigation.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.