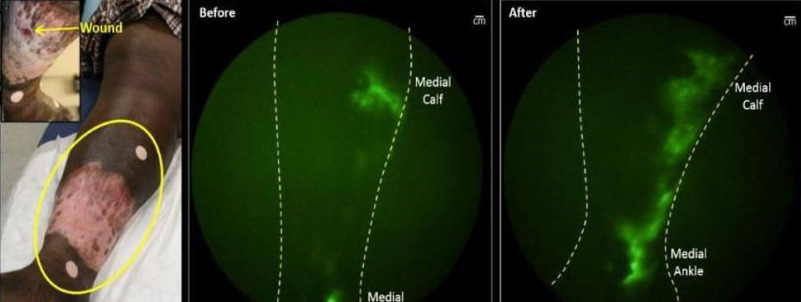
It’s interesting that patients are often less worried about their ulcerations than they are their edema, and in some ways it’s harder to treat. I am tormented by what we don’t understand about leg edema that we currently have the power to know. The US Wound Registry is a Qualified Clinical Data Registry (QCDR) that develops quality measures and reports data to CMS on behalf of practitioners subject to MIPS. It is a 501(c)(3) non-profit organization. The USWR was started in 2005 after CMS officials observed that it the reason wound care experts could not answer the most basic questions about the effectiveness of wound treatments was that they did not collect data in a standardized way. That wasn’t actually true. We had been collecting structured data on patients with wounds and lymphedema since 1997. In October of 2015, CMS made the switch to the ICD-10 diagnosis coding system which further improved our ability to collect granular data. Doctors who treat venous ablation are very interested in secondary lymphedema. Lymphedema is wildly under-diagnosed, even when it’s clinically obvious. I have previously posted images of the lymphatics acquired with an infrared imaging technique developed by Dr. Eva Sevick showing obvious lymphatic malfunction in a patient with venous ulcers (part of a larger study).
Clinicians caring for patients with venous insufficiency have known for years that they develop secondary lymphedema. There are a lot of factors involved. We know that 30% of patients with venous ulcers have diabetes and 70% are obese. Most are also hypertensive and are taking medications which can cause edema (e.g. calcium channel blockers). They also often sleep in chairs due to sleep apnea or heart failure, so the issues are complex. Out of curiosity I decided to tip a toe into the mysterious ocean of available data since October 2015 (remember, we have 10 years of registry data prior to that). Just since October 2015, there are 121,273 patients in the registry, of which 6,038 have been diagnosed with lymphedema (5%). In contrast, 34,165 patients have been diagnosed with “edema” (28.2%), making “edema” perhaps the most common co-morbid condition in the database. This may be the most important and overlooked problem that affects patients.
Just since October 2015, there are 29,498 patients with venous stasis or venous insufficiency which is 24.3% of all the patients in the registry. Perhaps most interesting, if you limit your search only to the 29,498 patients with venous insufficiency or a venous ulcer, 4,029 of them have been diagnosed as having lymphedema. It seems that at least 13.7% of patients with venous ulcers also have lymphedema, although I am confident that’s an underestimation. We could look at their leg photographs and see how many have lymphedema to the naked eye, and then we would have a better idea of the prevalence of lymphedema and the degree to which it goes unrecognized.
I’m suspicious that there may be a correlation between lymphedema and certain medications. We could figure that out since we have the electronic prescribing data on all of these patients. And, if anyone ever wanted to understand the effect of compression, we could do that since we have pre and post compression measurements and know every type of compression bandage, stocking or Velcro device (e.g. Farrow, Juzo, Circaid) that was used since many clinicians are reporting the USWR compression quality measure. I don’t have much hope that we will ever have the funding to answer questions about these mysteries, but, since it only took a few minutes to pull these data, I thought I’d share it with you.
The role of the lymphatics is underappreciated. Here’s a venous ulcer patient whose lymphatics were imaged with Near Infrared imaging. You can see that the lymphatics are severely affected. We see this every day in patients with venous disease.

Be sure to join me this week at the SAWC Spring conference. Get my full speaking / moderating schedule here.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.