Every time someone gives one of those “how wounds heal” lectures, it starts with “the first phase of wound healing is hemostasis,” and we think to ourselves, “Yeah, yeah, everybody knows that part . . .” Lately I’ve been paying more attention to the issue of hemostasis, or perhaps the lack of it. The US Wound Registry collects observations on the character of wound drainage as a structured field and the concept “bloody” was not used very often until a few years ago. Now it seems like a lot more patients have bloody drainage. I’m noticing this in my patients. They ooze blood even under their compression wraps. It’s not that they bleed because their dressings got stuck. You can see that the blood has been gradually oozing for days.
Out of curiosity, we looked at US Wound Registry (USWR) data to see what percentage of chronic wound patients were on anticoagulants or anti-platelet therapy (excluding aspirin). We only analyzed patients with wounds and ulcers from January 1, 2017 to November 27, 2018. There were 19,471 total patients of whom 9,700 were on an anticoagulant or blood thinner (19% of the total) with the distribution being: Plavix 6.9%, Coumadin 6.2%, Eliquis 3.8%, Xeralto 2.8%, Pletal 0.7%, and Pradaxa 0.5%.
Based on USWR data (at least since 2017), 19% of all patients with chronic wounds and ulcers are on anticoagulants or antiplatelet agents. I can tell you that the majority of patients taking anticoagulants have atrial fibrillation, although some have a history of deep venous thrombosis.
I can also tell you that I see a lot of bloody dressings. And lately, when I see dressings that stay bloody and wounds that aren’t making progress, I’ve starting putting products like Quick Clot into the wound bed.
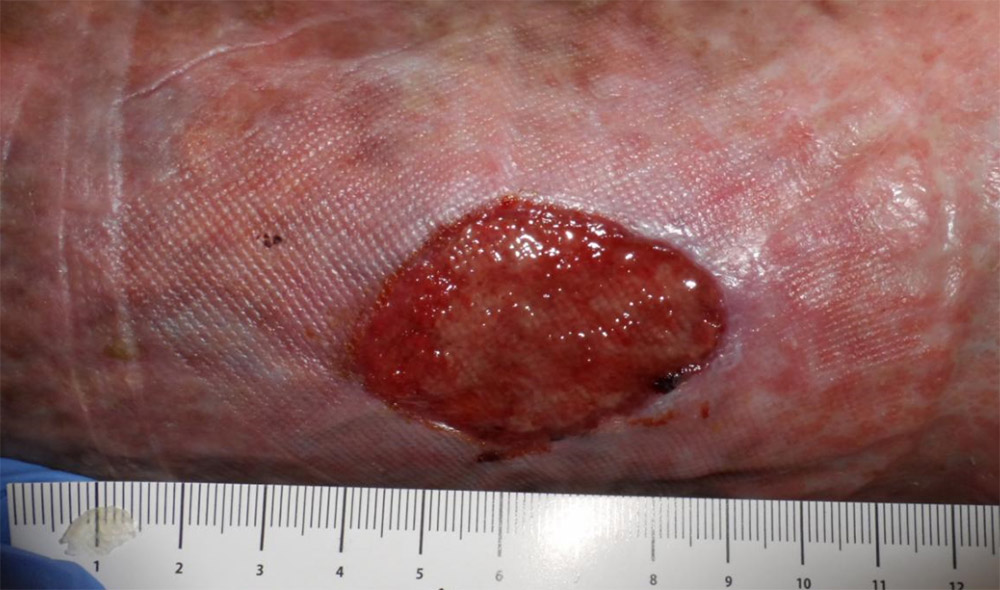
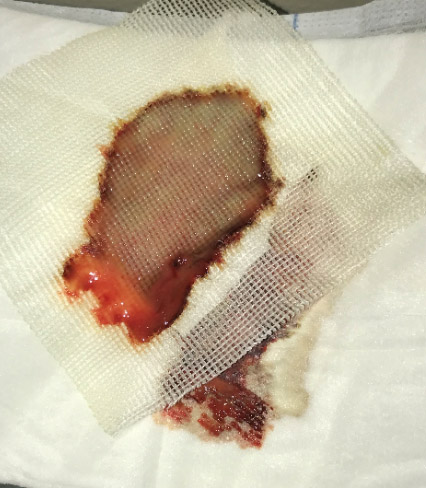
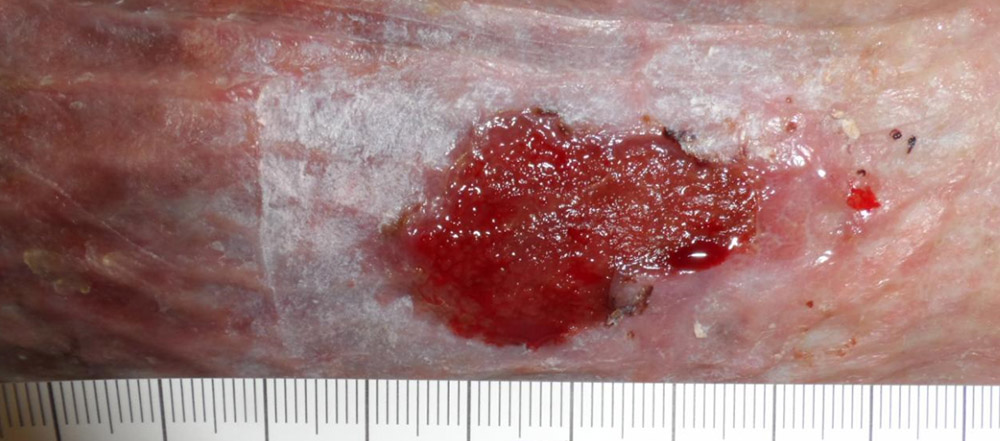
Here’s a patient with atrial fibrillation and some really refractory venous ulcers. He had been getting recurrent ulcerations for 3 years (he also had CHF). This particular wound had not improved for 2 months. You can see that the wound dressings under the compression dressing had red-black ooze. The next photo is the wound about a week later and the dressing which still is pink but not as bloody, and then 8 weeks later when the wound is clearly healing. I think the primary difference was that I was putting Quick Clot on the wound to stop the oozing.
- The wound in January.
- Late February – no improvement.
- Late February – red-black ooze on the wound dressing
- About a week later….
- …the dressing is still pink, but not as bloody.
- Eight weeks later – the wound is healing.
Has anyone else noticed this? We could figure out whether bleeding is an issue using USWR data, but it’s a “real world” problem and I don’t see anyone really wanting to know the answer to this, or whether there’s an association between slower healing and any of these medications.
Here’s a 9 second video of a patient on blood thinners whose granulation tissue just oozes. Yes, it’s true that granulation tissue is “friable” if it’s colonized but …uh… this is bleeding….
[vimeo 303280520 w=1080 h=1920]
Since the first phase of wound healing is hemostasis – I’m just observing that we may have a bleeding obvious problem.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.







i’m a patient taking eliquis and I have noticed this..nothing life threateneing ..but i always had “good skin”, good healing,,now a minor burn at the stove ..heals slowly..maybe permatently scared..and a cut that i wasn’t concious of getting..is obvious on my leg months ..later..i knew it was an issue after my ablation..which was successful and i am so grateful for the wonderful care i received …but the groin incission which did not bother me developed blood pooling (for lack of medical nomenclature..and though it faded over..time..it took at least 6 wks(or longer) before my thigh didnt look as though it had been in a major accident, and yes it was quite sore..but not a big deal….eventually it faded leaving a faint maping at the sight..almost 8 months later it is still there..so yes..i noticed and i was certain it was the blood thinners..having had a blood clot in my heart a couple of months prior to the ablation…I take my eliquis..faithfully..
My brother who is on Eliquis for DVTs is now in wound care for his incision for recent back surgery. Infections with IV antibiotics haven’t helped and the wound continues to seep and keep him hospitalized