I recently saw a patient with digital ischemia who got improvement in both pain and tissue viability with transdermal oxygen from the OxyBand dressing. There are a lot of possible reasons for digital ischemia, so it’s important to know why the patient has ischemic fingers. I can’t do justice to the topic here and don’t want to pretend that I have a lot of expertise other than seeing a lot of these. However, you can’t treat a patient effectively until you have determined whether it’s due to the flare of an autoimmune disease that needs controlling, whether spasm is the primary issue, whether the problem is rheologic, whether they have vascular disease, Burger’s or some combination of the above. Stopping smoking is a given, assuming you can make that happen. With the caveat that this is a huge topic, I wanted to do poor justice to it because I thought I’d mention a basic toolkit that I use, and the fact that, to my surprise, the OxyBand transcutaneous oxygen dressing gave the patient considerable relief of pain and visible improvement.
I was asked to see the patient because he was waiting for is insurance to authorize hyperbaric oxygen therapy, a process which took several days and during which time his left middle finger went over the edge and it was too late to save the distal tip. That’s why I thought it would be good to talk about an emergency toolkit since it’s getting harder to get HBOT for anyone.
The patient in these photos has CREST, also known as limited scleroderma. CREST is an acronym for the clinical features that are seen in a patient with this disease, specifically:
(C) – Calcinosis: calcium deposits in the connective tissues
(R) – Raynaud’s phenomenon: where the hands and feet turn white and cold and then blue, and can even become ischemic (usually in response to cold but also to other factors)
(E) – Esophageal dysfunction resulting in swallowing difficulty
(S) – Sclerodactyly: thick and tight skin on the fingers, caused by an excess of collagen deposits within skin layers.
(T) – Telangiectasia: small red spots on the hands and face that are caused by the swelling of tiny blood vessels.

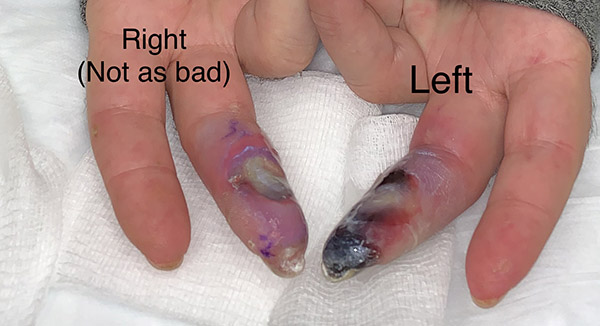
He got dramatic improvement in his digital ischemia with application of the OyxBand dressing. Perhaps the most striking feature is that he got a lot of pain relief from the dressing which seems important. It’s clear from the photos below that the left middle finger was in worse shape to start with.

After 72 hours of the OxyBand, the edema of the finger is dramatically reduced and that’s what’s causing the skin to peel. In a week, the finger is beginning to demarcate.
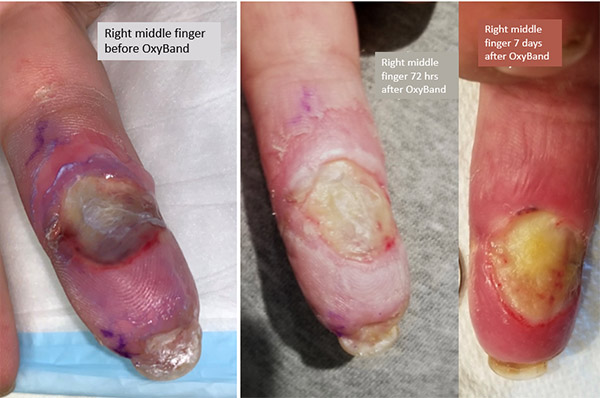
The improvement of the right middle finger was dramatic after 72 hours and after a week there may even be a few granulation tissue buds at the base of the ulcer.
Here is a movie of OxyBand being applied to the finger, from my YouTube channel:
This patient’s situation made me think about some issues that I think are deserving of comment.
Thankfully we normally only see one case like this a year. That means that a patient who has digital ischemia with threatened gangrene of the fingers has some serious problems that are not strictly medical, including:
- They may be the first patient like this that their doctor has ever seen.
- The doctor(s) may not understand that even when the digital ischemia does not appear severe, interventions must be started NOW because it will be too late if you wait until the need for an intervention is obvious.
- There are a lot of “tricks of the trade,” and sometimes it is better to have several small interventions than one big one that might not work and comes too late because you had to wait a week to start it (e.g. hyperbaric oxygen therapy).
- Reductions in flow can be multi-factorial – patients can have both vascular disease AND spasm. Addressing several mechanisms is a good plan.
- They may be the first patient like this the payer has dealt with and they are outside the usual decision trees.
- The payer doesn’t know it’s a “slow-moving” emergency with ischemia progressing over 24 to 48 hours.
- The payer is going to put them through the usual authorization process, which means the work up and interventions they need won’t get approved for at least a week, by which time it will be too late.
- These patients should be hospitalized, or they won’t get the care they need in time.
I was asked to see the patient for a second opinion because they were waiting on authorization to start HBOT at a facility that was closer to their home. I should issue a disclaimer that I’m not a rheumatologist and have no special expertise in connective tissue diseases. However, I do have some rules that have stood me in good stead when it comes to patients with mixed connective tissue disease and ischemia:
- Do not sharply debride any lesion on their fingers or toes. It will make them worse. Period.
- Get an angiogram unless there is a compelling reason not to do so. I screen all my patients with skin perfusion pressure, and I can even use a digital cuff to get the digital PVR and perfusion pressure, but the basics are still the basics; find out if they have normal large vessel flow. I do understand that they may be having a spasm, but when the goal is to save fingers, increasing the pressure head may be necessary.
- Address the underlying disease. If it isn’t clear whether their disease is “flaring” – treat them as if it is. You can argue the fine points later if they can still use a computer keyboard when it’s over. No one ever looks back on these cases and says, “Gee, I overreacted and gave them too much care.” Every regret you will ever have with these patients will start with, “I had no idea they were in this much trouble.”
- Have a Digital Ischemia Toolkit. Here is mine. I am sure that many readers have more expertise than I do and can make better recommendations than this. There aren’t a lot of articles about the “tricks of the trade” for ischemic fingers – or if there are, then I missed them:
- Pharmacological therapies to improve blood viscosity:
- Aspirin: Unless there’s a reason not to take it, a baby aspirin per day (81 mg).
- Pentoxifylline (Trental): The original drug used for claudication. It’s been replaced by Plavix for claudication, but has reasonable data for the treatment of venous stasis ulcers. It may improve flow by improving viscosity and some say it has an anti-inflammatory effect, but I am not sure about that. It’s very safe, usually very well tolerated, and doesn’t actually cause bleeding like anticoagulants.
- Pharmacological therapies to improve blood flow:
- Clonidine Patches: Its mechanism of action to reduce blood pressure is peripheral vascular vasodilatation. It comes in several doses and is usually well tolerated. Even in patients with normal to low blood pressure, I’ve not had problems with orthostatic hypotension. Patches have the advantage that if they make the blood pressure drop too much, they can just be removed. They are placed on the chest, not the extremity, and the active drug is a kidney metabolite so it’s no use in patients on dialysis.
- Cialis or Viagra: Insurance usually limits the patient to about 9 tablets per month. Cialis has the advantage of being longer-lasting than Viagra. The mechanism is via its effect on Nitric oxide to vasodilate.
- Beta Blockers: Amlodipine is used up to doses as high as 20 mg/day.
- SSRI’s (Depression Medication): Selective serotonin re-uptake inhibitors.
- Pharmacological therapies to improve blood viscosity:
Other Treatments That Can Vasodilate:
- Anodyne Therapy: Near infrared light which activates nitric oxide to dilate the vessels. It’s topical and safe, except I did have a patient get burned from the heat of the pads when they fell asleep with the pads on. Treatment only takes a few minutes. I tell patients to set a timer. It is not covered by insurance. The last time I checked it was about $300 per month and patients can buy a refurbished unit, but don’t hold me to any pricing because I haven’t tried to keep up.
- Heat: Gel mittens or socks that you can heat in the microwave can be used with CARE – you have to know the microwave and have someone test the heat after a certain number of seconds. However, the advantage of the gel mitts or socks is that they will only cool off over time, as opposed to a heating pad which can continue to get hotter and then burn people when they don’t realize it.
Hyperbaric Oxygen:
HBOT can raise tissue oxygen levels, but it actually causes vasoconstriction of the arteries. It doesn’t improve pain that much in my experience, even when it saves tissue.
The Nuclear Option for Digital Ischemia:
- The last option is IV Flolan: We use this if there is threatened loss of digits from vasoconstriction. It requires hospitalization. It will dilate the vessels, but it will cause a horrible headache that may require narcotics. As a migraine sufferer, just thinking about it makes me nauseated, but I’d rather have a migraine than lose my fingers.
- Rheumatology at my old institution would start Flolan intravenously at 2 mg/kg/min, checking vital signs every hour on some unit that could provide really close monitoring. The patients needed IM Phenergan and oral Vicodin, and their vitals were checked hourly during titration. The infusion was increased every hour by 0.5 mg/kg/min to a max of 6mg/kg/min until the patient’s headache was so severe it couldn’t be controlled with Vicodin, they couldn’t stop vomiting, or their systolic BP dropped below 90 mmHg. At that point, the Flolan dose was reduced by 0.5 mg/kg/min until the headache, vomiting or BP improved and that dose was then used as the maintenance dose. The patient was kept on the maintenance dose for 2 to 4 days with vital signs every 4 hours at that point. I’m not giving medical advice, I’m just telling you the way the protocol was performed.
OxyBand Dressing:
I confess, I did not think this would work, but not only did transdermal oxygen improve the ischemia of the fingers, it dramatically reduced the pain.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



