Mysterious Sepsis in a Dialysis Patient
I have been taking care of a young woman with Type 1 diabetes who lost her kidney transplant about a year ago. She suffers from all the complications of diabetes, and is on home peritoneal dialysis. When I first saw her, she had a large abdominal wound from one of her many transplant-related surgeries which had been open for months. I decided that the problem with her abdomen was simply that she was malnourished. She told me that she had been in the hospital twice with sepsis in the past 6 months, the source of which remained a mystery. Getting her on vitamins and a lot more protein healed her abdomen. She also had a left heel pressure sore complicated by peripheral arterial disease, but even that improved significantly with better nutrition. I was feeling good about her progress, and then once again, she became septic, presenting with sudden left leg pain, swelling, and the rapidly-ascending erythema characteristic of a necrotizing infection. The transplant team performed fasciotomies of the lower leg and opened her left medial thigh to drain what appeared to be an abscess. Her muscle was perfectly pink and only clear fluid was found in the thigh, which showed no growth on culture (see the photo below). She was sent back to me as an outpatient to manage her very large post-operative wounds with NPWT.

On one of her fist NPWT changes, we managed to access a persistent fluid pocket in the left thigh. The fluid was clear and odorless. She was already on intravenous antibiotics, so I sent the fluid for DNA sequencing. (We use MicroGenDx). Using DNA sequencing information in a reasonable way means taking the results in context with the patient and the wound. It generally takes 10 days for the final report, which is not a big problem if the goal is to understand a persistent biofilm. If the patient has an acute infection, it’s still better to do a traditional culture so you can have antibiotic sensitivities.
Although her wounds continued to look better with NPWT, she didn’t look better. A week later the left thigh wound had grey/black tissue that appeared to be necrotic:

However, unlike necrotic tissue, it could be removed with a Q-tip:

All day I had the feeling that I was forgetting something. The next day, I received the MicroGen report. Here’s the important part of an extensive report:
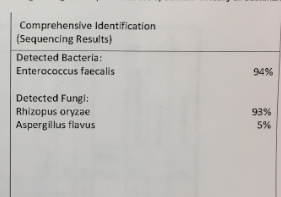
DNA sequencing had detected Rhizopus – also known as mucormycosis. And then I remembered! I had seen in in about 1992, not long after opening the hyperbaric facility in the Houston Medical Center:
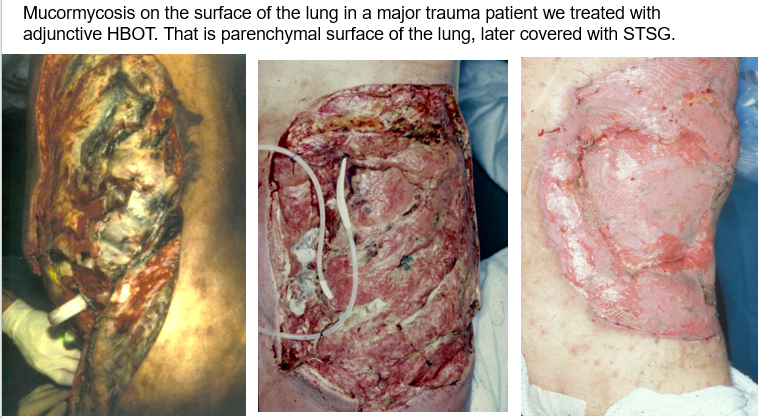
The photo above is poor quality because I took it with a Polaroid camera. The patient had developed a traumatic empyema in a motor vehicle accident, which became infected with mucormycosis.
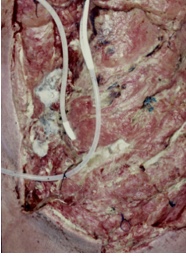 The material on the pleural surface of the lung (right) looks like bread mold. He was treated with hyperbaric oxygen therapy and actually recovered. Eventually skin grafts were placed directly over the granulated pleural surface.
The material on the pleural surface of the lung (right) looks like bread mold. He was treated with hyperbaric oxygen therapy and actually recovered. Eventually skin grafts were placed directly over the granulated pleural surface.
Mucormycosis is a serious but rare fungal infection caused by members of the order Mucorales, fungi found in soil and in association with decaying organic matter. The species that most commonly cause mucormycosis are Rhizopus, Mucor, Apophysomyces, and Lichtheimia. The spores are often inhaled, which is how they cause Rhinocerebral mucormycosis, an infection in the sinuses that can spread to the brain. I have treated several diabetics with HBOT for this awful infection, but when mucormycosis is in the sinuses or brain, you don’t actually SEE the fungi. Pulmonary mucormycosis most often occurs in cancer and transplant patients. Cutaneous mucormycosis can develop when the fungi enter the body through a break in the skin. I don’t want to pretend to be an infectious disease doctor, so I won’t discuss treatment or prognosis.
For this patient, I immediately raised the alarm with the transplant team. She had probably had this infection for months, and it was likely the cause of her recurrent and unexplained episodes of sepsis. I felt bad that I hadn’t figured it out 4 days earlier when I saw that greyish material in the thigh wound, but the transplant team was just grateful to finally have an answer. I knew that I had seen the strange material inside her wound somewhere before. It turns out that it had been more than 25 years earlier. I wanted you to see it, so that if you encounter one of these sad cases, you won’t miss it.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



