I started this series of blogs with a discussion of Medicare audits and the impending bankruptcy of Medicare. We determined that audits come from perceived improper use and the reason that audits are accelerating is the impending bankruptcy of Medicare. Medicare is running out of money because the cost of caring for patients is more than needed to provide quality care. We are overspending for the quality of care we provide based on Medicare spending per beneficiary. If HBOT or any other modality does not decrease spending per beneficiary, then it doesn’t “work” in a way that Medicare or the private payers care about. I used to feel uncomfortable with the idea that “it’s all about the cost of care.” But, truthfully, if we really make someone better, spending on their conditions will go down. Spending is a surrogate for outcome.
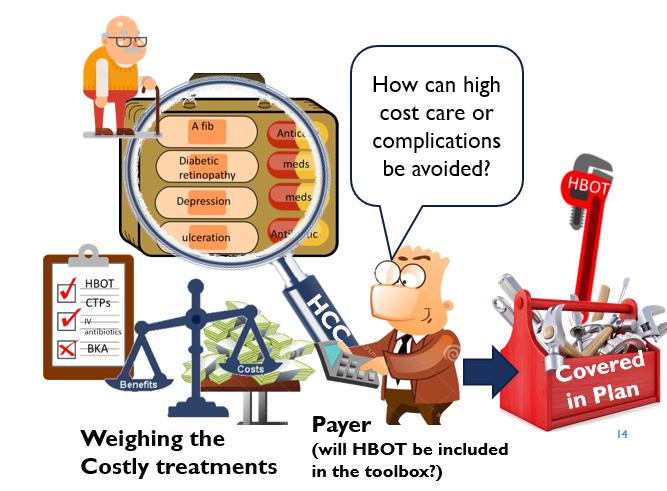
As you can see in my illustration below, the payer sees the patient through the lens of his co-morbid conditions and associated costs to the system. The lens through which Medicare views “illness” is the HCC score. If payers (Medicare or private) believed HBOT or any other advanced therapeutic decreased overall spending, they would pay for it regardless of whether it had an RCT. In fact, if payers believed that an intervention improved quality and reduced cost, they would probably mandate its use.
Key Point: We now understand is that it is not enough that a treatment “works” clinically for symptom improvement. We must be able to show that Medicare spending decreases when it is included in the toolkit. This may be evidenced through a reduction in Medicare Spending per Beneficiary, a decreased likelihood of hospitalization, or a reduced risk of amputation (as only 3 examples).
3 things can you increase your chances of survival right now:
- Use the UHM taxonomy for all physician claims (even if you perform very little HBOT, in the absence of a taxonomy for wound care, at least you would be compared to a group of practitioners with equally sick patients and thus similar MSPB).
- Achieve high scores on the quality component of MIPS. That gives you the best chance at the “value” tier. The best way to do that is reporting through a Qualified Clinical Data Registry.
- Document to ensure the best possible HCC scores, which will help explain your MSPB
The Roadmap for survival of the field:
- Participate in the US Wound Registry (a QCDR) to optimize your quality scores and enable the USWR to establish the average HCC score for the subspecialty of hyperbaric medicine.
- This would help physicians end up in the optimal tier for the value modifier and that equates to revenue.
- Ensure there is a hyperbaric physician member on every episode of care committee that CMS is creating.
- Fund analysis of the MSPB for key HBOT conditions so we can determine whether and how HBOT might be decreasing overall cost.
- It is hard to use claims for some of our applications because the diagnosis codes might not be used properly or even characterize the condition (e.g. there is no ICD-10 code for a diabetic foot ulcer).
- Analysis might have to be linked directly to the patients in the USWR to make sure we have the right patients in the treatment arm.
- If we are not able to show that HBOT decreases spending, we won’t be able to keep it and perhaps we shouldn’t.
- Improvements in total spending might not be exactly what we think they are (e.g. decreased rate of hospitalization or cellulitis)

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.