An increasing percentage of my wound center patients have Medicare Advantage plans offered by private payers. As I’ve discussed on previous blogs, it’s getting very hard to use cellular and/or tissue-based products (CTPs) on chronic wound patients with Medicare Advantage. Assuming you make it through the prior authorization (which may require a “peer to peer” phone call with the payer), you then have to figure out what product you can use.
I’ve blogged before about the issue that the private payer may limit coverage to a specific CTP that I don’t have available in my wound center (sometimes by our own choice based on decisions driven by the cost constraints of “package pricing”). I once complained about this personally to a CMS official at Medicare headquarters in Baltimore who told me that as long as the payer covered “something,” then they met the Medicare requirement. Since then, I have an attitude of “learned helplessness” when it comes to CTPs in Medicare Advantage patients. This doesn’t seem right, so I’ve been trying to better understand the rules surrounding Medicare Advantage and CTPs. I’m not a certified coder or biller and I don’t offer that kind of advice. I’m a doctor in the trenches trying to Do The Right Thing for my patients. I’m providing information as I understand it. If some of you have better information, I am grateful to know it and will try to share it.
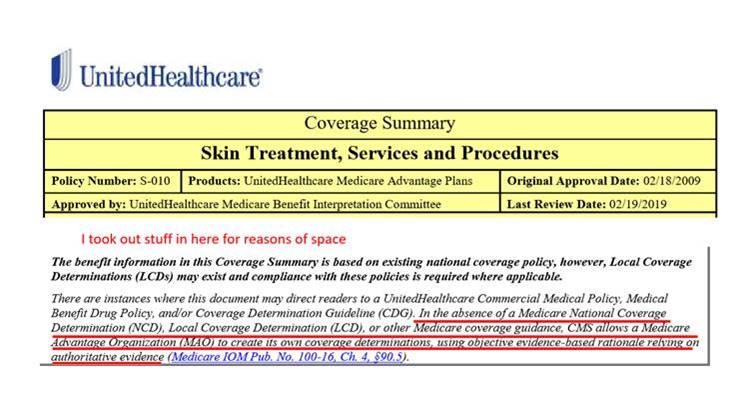
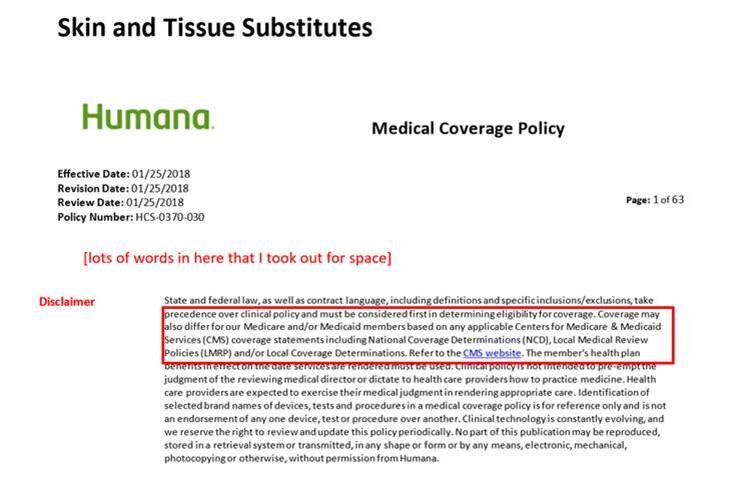
In order for a company to contract with Medicare to provide Medicare Advantage (“Medicare Replacement”) plans, they must provide at minimum the same level of coverage as Medicare. This means that the commercial payer must follow all National Coverage Determinations (NCDs), as well as any relevant Local Coverage Determinations (LCDs), if they exist.
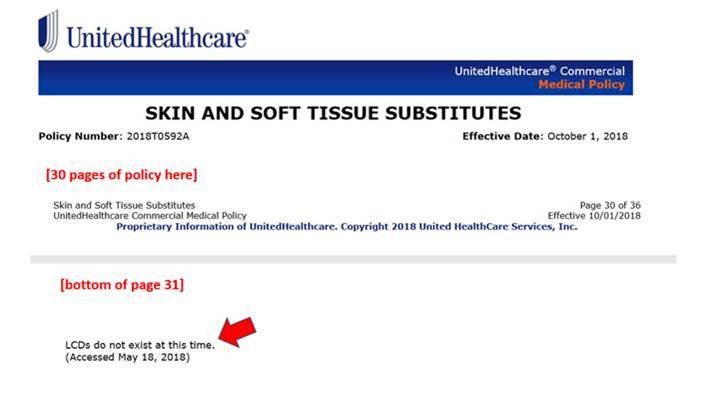
We’ve recently seen several commercial payers release their own policies pertaining to Cellular and/or Tissue Based Products (CTPs). These commercial policies list the CTPs the payer does/does not cover. However, at the very end of each policy is some fine print stating that in those regions where an LCD exists on CTPs, they follow the LCD [when administering Medicare benefits]. That means that in a region where the Medicare Administrative Contractor has no LCD on cellular products (or the LCD has been retired), the commercial payer administering Medicare Advantage reverts to its commercial coverage policy. The language the private payers use is something along the lines of (and I am totally paraphrasing), “We do cover CTPs for our Medicare Advantage beneficiaries, so we are providing the same ‘level of coverage’ as Medicare- we just limit our coverage of CTPs specifically to products X and Y. And, it’s totally OK for us to make the decision to limit them, because the CTPs we cover have scientific evidence in the form of randomized controlled trials while the others don’t, so we are basing our decision on science.” Remember the above is totally my paraphrase, but I think that conveys the gist of what they say. Nevertheless, if that same patient had a traditional Medicare fee for service (FFS) plan instead of a Medicare Advantage plan, practically any CTP would be covered.
To summarize, in a region with an active LCD on CTPs, the private payer offering the Medicare Advantage Plan must follow that LCD, regardless of how restrictive their own private payer policy might be. If there is no active LCD in the region, then the private payer reverts to its own company policy on CTPs, which most likely limits “Medicare coverage” in their plan to one or two products.
What I am trying to convey is that if you live in a region with an active LCD on CTPs and a Medicare Advantage plan denies the product you wish to use, you can appeal their decision, citing the “fine print” that the private payer must follow an LCD if it exists when administering Medicare Advantage benefits. (Naturally private payers can do whatever they want when it comes to the beneficiaries within their own commercial plans.) Many CTP manufacturers offer benefits verification programs and will assist you in appealing denials (for their product) if a commercial payer is subject to an active LCD which would otherwise cover it.
Medicare Administrative Regions and LCDs on CTPs
| MAC | Policy |
| CGS | Active L36690 |
| Palmetto | Retired 01/2019 |
| First Coast | Active L36377 |
| NGS | Retired 09/2016 |
| Noridian | Retired; Cover Articles on Amnions and Wastage |
| Novitas | Active L35041 |
| WPS | Retired 03/2016 |
Here are some snips I took from various policies demonstrating the language (click on the image to zoom):

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




Great article