Guest blog post by Dr. Helen Gelly
Using the claims data from Medicare that are publicly available, a newly published study which I co-authored looked at various parameters that will eventually impact the bundled pricing payment model. Because a number of insurance carriers have limited the availability of cellular tissue products for clinical use, it was important to explore cost, wastage, frequency of applications, and impact on amputation in this vulnerable population.
Here’s a link to the article: https://pdfs.journals.lww.com/aswcjournal/9000/00000/The_Health_Economic_Impact_of_Living_Cell_Tissue.99937.pdf
The cost of care for chronically ill patients is an issue of increasing concern and payer scrutiny. Wounds are a chronic health condition. Wound care patients are often in service for over 6 months, and we try many different modalities to get them to heal. As some form of “bundled payment” for wound management becomes more likely, it is critically important for us to have data on what we do to care for them. Unfortunately, most published studies are limited to a few practice sites that mandate compliance to a protocol (which is darn near impossible to achieve on a scale). Randomized, controlled trials, seen as the gold standard, exclude so many conditions that the results only apply to imaginary patients that are not too sick and who have only one wound that is not too bad.
Despite its limitations, looking at Medicare claims data gives us an idea of how we practice as a group, what products we use, and how often we use them on the real patients we actually SEE. Medicare claims provides insight into the practice patterns of thousands of clinicians and tens of thousands of patients. We can look at relative costs, some outcomes, and compare typically expensive products, both for utilization as well as frequency of application.
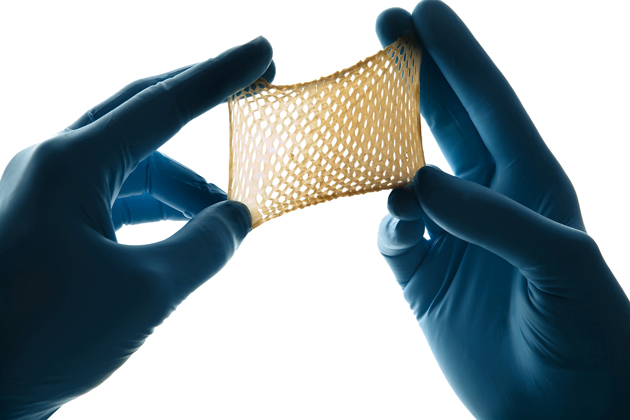
We know that Medicare expenditures related to wound care are far greater than previously recognized. Medicare beneficiaries receiving cellular tissue-based products (CTPs) represent a unique subset of patients that have failed conventional care. Living cellular tissue products have been proven to be superior to standard care alone, but little is known about their relative cost-effectiveness in the real-world setting.
In this study, we analyzed Medicare claims from patients who received either TheraSkin, Apligraf, or Dermagraft and matched the groups by Charlson Comorbidity Index (CCI), age, gender and region. The study demonstrates that wound-related costs, product waste, amputations, and frequency of applications are lower for TheraSkin than Dermagraft. Wound-related costs and product waste are lower for TheraSkin compared to Apligraf.
Further claims analysis and prospective real world clinical trials could help develop appropriate quality measures and reimbursement models to ensure smarter Medicare spending for this growing population. More studies like this are needed if we hope to maintain access to advanced therapeutic modalities for wound care patients. Treatments have to make sense both clinically and financially.
Helen Gelly, MD, FUHM, FACCWS, UHM/ABPM
Hyperbarxs

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.