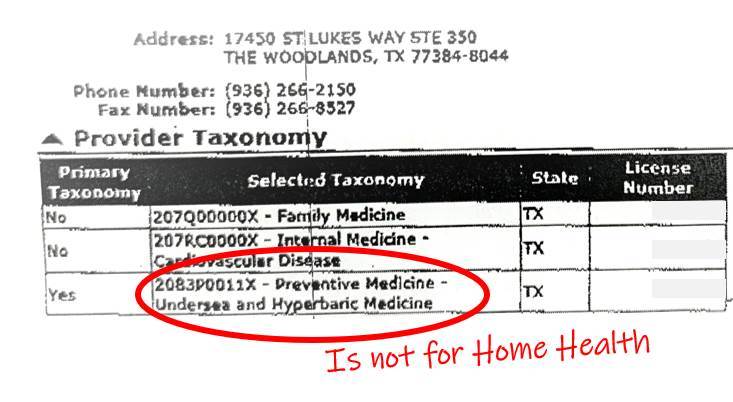
I changed my specialty code to Undersea and Hyperbaric Medicine a few months ago. It was necessary because since I am Family Practice Board Certified, the data on Medicare spending for my patients was being compared to that of FP’s across the country. However, I see much sicker patients than the average FP and use a lot more expensive treatments. Without a specialty code for “Wound Management,” Medicare just assumes I am an overspending FP who can’t keep heart failure patients from being readmitted to the hospital.
As I have discussed before, the lack of a Wound Management specialty code WILL be the death of wound management services practiced by physicians – at least those with a primary care board certification. The best way forward for me was to change my specialty code to Undersea and Hyperbaric Medicine. It’s a logical change since I do practice hyperbaric medicine, even if I spend most of my time as a wound management practitioner. However, I think that even wound management practitioners who DO NOT practice hyperbaric medicine should change their specialty code to Undersea and Hyperbaric Medicine if they want to survive healthcare reform.
I can now confirm that that Medicare knows I practice UHM rather than Family Practice, at least, I THINK they do… I have not seen my Medicare spending report since I made the change in specialty code, and I can’t tell you whether this plan will work to save the field. However, changing my specialty code has impacted payment for Home Health services for my patients.
Here’s the bullet point version:
- About 25% of patients I see in the wound clinic are also receiving skilled Home Nursing services.
- Usually, I fax the dressing change orders to the patient’s PCP so that he/she will sign the Home Health Agency’s “485” form.
- The Home Health Agency expects the physician who signs the 485 to assume responsibility for all the patient’s care plan, including medications I don’t prescribe and conditions I don’t treat.
- I used to just sign the forms anyway, but stopped after serving as a defense expert for a wound care doctor who was sued over a patient’s Coumadin orders which were included on the Plan of care for dressing changes.
- I try to give all my patients the same high quality and loving care, but I confess, there are some patients who make an impression. One of my “fav patients” is a man with an above the knee amputation of one leg and bad lymphedema with open wounds on the other leg. He’s engaged in a life-long battle with his lower extremities, but no matter what, he’s always cheerful and it’s an honor to be his doctor. It is so hard for him to get into his primary care doctor’s office that I made an exception and for months have been signing the 485’s for his Home Nursing services.
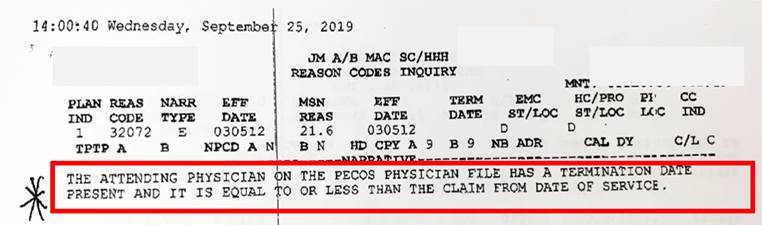
- Today someone from his Home Health Agency called my office, furious that they had not been paid by Medicare for several months. The reason had to do with the change in my Specialty code (Provider Taxonomy). When I changed my provider taxonomy, the Home Health agency stopped getting paid, although they only just realized it this week.
I have included the Ordering/Referring Physician Checklist for Home Health Agencies. It is pretty clear that the Home Health Agencies are responsible for checking this list regularly for updates.
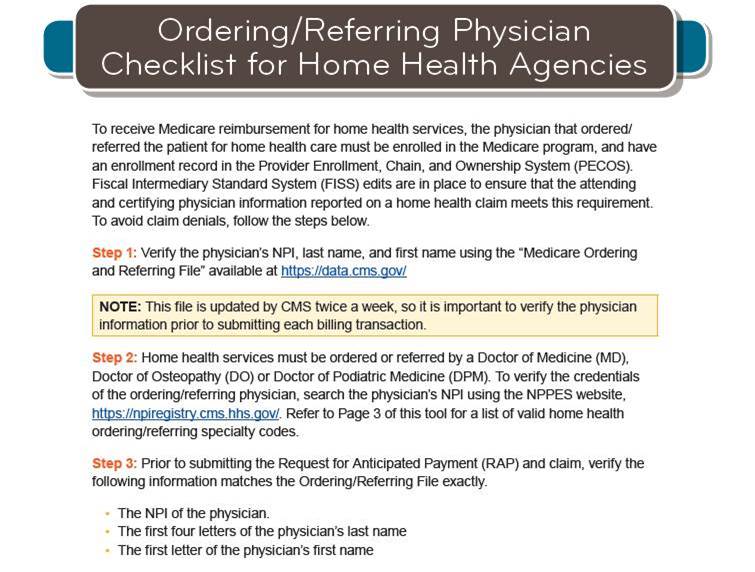
While the Bad News is that the Home Health agency may not get paid for services they provided (and they have done a great job caring for him), I thought the GOOD NEWS was that it meant Medicare had gotten the message I was not a family practice physician. The answer is not so simple. According to this CMS report, I am still listed as a physician who can sign Home Health Orders. That may be BAD NEWS, because it may mean CMS still holds me responsible for their re-hospitalizations.
Here’s a screen shot of the CMS report showing that I am still able to sign Home Health Orders (just like 6 other physicians with my unusual Scottish last name who are probably long lost cousins).
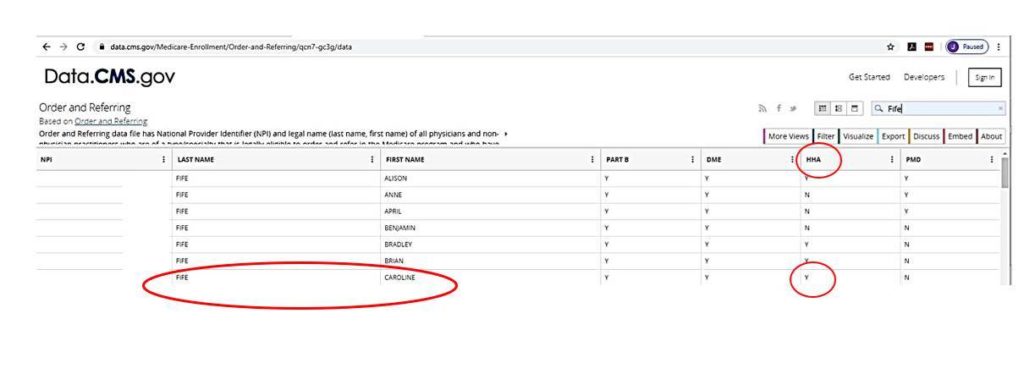
So, now I am really confused. I have confirmed that Medicare knows the specialty I practice is Undersea and Hyperbaric Medicine. One CMS database says I can sign home health orders (linked to my NPI) while another database (updated regularly by CMS and linked to my specialty code) indicates that I can’t. The latter CMS website indicates that I can also sign orders for Durable Medical Equipment (DME). If that’s the case, why can’t DMEs accept prescriptions signed by me for diabetic shoes, instead of holding the process up for weeks/months to get a signature from the PCP?
I had long ago decided not to accept the liability of signing the Home Health Agency 485 – at least, for all patients except this one. It turns out that it wasn’t really a favor for him, because now his Home Health services are threatened. Since I contact the patient’s PCP anyway and send them follow up letters, I might as well get the PCP involved in signing the 485. That means my NOT signing the 485’s won’t be a change for me as an official specialist in UHM. I suspect some of you have been signing 485’s for your patients, so NOT being able to do so might impact your willingness to change your specialty code. I think you had better check your MIPS data when it is made available. I don’t think we can afford to be mistaken for PCP’s, and not being able to sign Home Nursing 485’s is a small price to pay for our survival as a field.
In the meantime, if you have any insight into other impacts of using the UHM specialty code, please contact me and I will make sure your information is added to this post.
Useful Links:

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




Caroline, I am so very grateful for your energy and intelligence in all this. I must confess, this all feels like way too much for me on many levels and it truly makes me want to throw in the towel and “retire” early. In other words, run from this overwhelming mess. When I see that even you are confused, I see no hope for me to figure this all out. I too am FP/UHM