Here’s a guest blog from a friend and colleague who practices Undersea and Hyperbaric Medicine and is also a Critical Care physician. I believe that she should remain anonymous for now. However, I was inspired by the emails and texts she has sent me and thought you would be, too. She’s sending me messages off the cuff – they are “raw” and not edited by her. However, I think that is best. She uses a lot of abbreviations and when I thought it was useful, I explained them in brackets. One day at the right time, I will tell you who she is and we can all thank her properly for her courage and commitment. Here are her COVID-19 Diaries – uncensored.
–Caroline
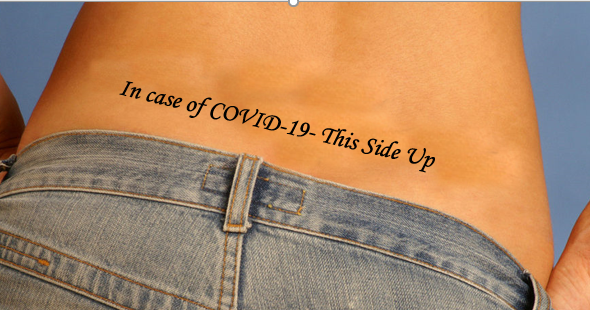
COVID-19 Diaries – This Side UP
I’m pondering the things I have learned so far. These are sort of random thoughts.
Explaining the GI symptoms in COVID-19
There tend to be these 2 different presentations – one with more GI symptoms (like diarrhea) and the other with terrible pneumonia that leads to ARDS. The receptors for the virus are called “Ace-2” receptors (Angiotensin-Converting Enzyme 2). The tissues with the highest Ace-2 receptors are the lung, then the endothelium [blood vessel wall,CF], followed by GI tract. The characteristic “spikes” that cause it to be named the “crown” (aka coronavirus) act like a key and the Ace-2 receptors are the lock the spikes fit into. That’s one reason the first symptom might be anosmia (the inability to smell). That’s the virus binding the receptors of the nasopharynx as it makes its way down to the lungs. But about as many patients have nausea and diarrhea as those who have anosmia.
Is Gastric Reflux a risk factor for COVID-19?
It raises the interesting question of whether gastroesophageal reflux disease (GERD) plays a role in the most severe presentations of the disease, because it would facilitate viral particles moving from the gut into the trachea (although I am not sure they need HELP to do this). Anyway, I don’t know if GERD is a factor but 3 of my 4 sickest patients were very overweight. We’re also picking up perhaps some undiagnosed sleep apnea as their oxygen saturation is worse at night. Still, even thin patients tell me that breathing at night is worse. My doctor colleagues who are fighting COVID-19 all say all the nights are bad, with myalgia and struggling to breathe. In some cases we have them on maximal non-rebreather face masks AND nasal cannula oxygen at the same time. We are doubling up because they are breathing so fast they can over-breathe the delivery systems and suck in air around the masks. They need every molecule of oxygen they can get.
Keep This Side Up
I just watched the JAMA podcast with the U. Pitt critical care chief saying delayed intubation may be better than early intubation, and proning [lying face down, CF] on non-rebreather face mask oxygen might be the best management option. We are all learning the hard way – by our own experience with this disease, yet everyone seems to be seeing the same things – which is fascinating!
I am thinking of getting a tattoo on my backside that reads, “In case of COVID-19, keep this side up,” to make sure whoever takes care of me knows about prone positioning. (I might also get “DNR” tattooed on the front of me, because that’s a realistic assessment of the situation we face…)

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.