Wounds are a symptom of disease and usually the first disease we have to rule out in patients with lower extremity wounds is poor perfusion. Arterial disease is the most common reason but not the only one. I rely on skin perfusion pressure (SPP) to determine whether the perfusion specifically to the area of the wound is adequate. I am going to post a series of articles explaining why I must have this machine or I can’t provide adequate care.
–Caroline
Because you can’t trust Arterial Dopplers, especially in Diabetics…
Wounds are a symptom of disease, and usually the first disease we have to rule out in patients with lower extremity wounds is poor perfusion. Arterial disease is the most common reason, but not the only one. I rely on skin perfusion pressure (SPP) to determine whether the perfusion specifically to the area of the wound is adequate. I am going to post a series of articles explaining why I must have this machine or I can’t provide adequate care.
It seems that the other wound centers in my hospital system rely on the arterial brachial index (ABI). I am going to explain why that’s just not good enough, and I am going to show you why with examples of patients, starting with this one:
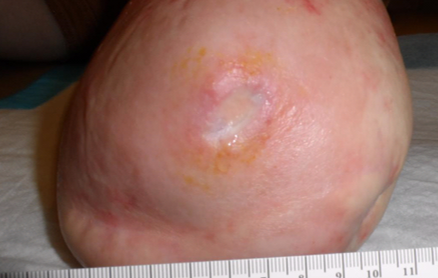
This is a 59 year old diabetic who lost his left leg below the knee 7 years ago after he stubbed his toe and developed osteomyelitis. He had been walking with a prosthetic limb until 3 months ago, when he developed an ulcer on his left lateral stump. He underwent surgery for a stump revision a month later, and that didn’t heal. Arterial Dopplers suggest that he has adequate perfusion to the stump. He’s had a variety of wound care treatments, but nothing is working and there’s no granulation tissue in the wound bed. On his first visit to the CHI St. Luke’s Wound Center in The Woodlands, Texas, I performed skin perfusion pressure. That’s a CMS-recognized quality measure, to perform an assessment of perfusion for healing potential on the FIRST VISIT, and frankly, I don’t think a place should be called a “Wound Center” if they can’t do that. Turns out his SPP was only 10 mmHg and there is a monophasic pulse volume recording (PVR). In other words, he has arterial disease and that’s why he got an ulcer in the first place after several years of doing well.
He underwent endovascular revascularization and he healed.
What do we learn from this:
- Arterial Doppler’s are not much use in diabetics to assess wound healing potential (and “ABIs” are of no use when you don’t have an ankle)
- A lot of healthcare money gets wasted because perfusion isn’t evaluated (he had a failed operation and months of futile care)
- Hospital cath labs benefit when the outpatient wound center can measure skin perfusion pressure
Stay tuned.
–Caroline

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



