We see a lot of sad situations in the field of wound care, but every now and then, a case really gets to you. This patient is a 47 yo man with a sacral pressure ulcer which had developed 2 months earlier when he was hospitalized for pneumonia. He suffers from a rare, progressive and universally fatal genetic neurogenerative disorder. In a few years he had gone from being a vigorous, physically fit man to a wasted, bedridden individual unable to speak (but alert mentally), with a body mass index (BMI) of 19. He had a tracheostomy, but the family had decided not put in a feeding tube. He had lost at least 40 lbs. He was lovingly cared for at home by his wife and a caregiver. On his initial examination, bone was visible in the wound which undermined 2.7 cm circumferentially. He was on an appropriate support surface, bacterial colonization was well controlled, and the wound was being treated with advanced dressings. The glaring issues was his nutrition.
I emphasized the importance of optimizing his nutrition as much as possible under the circumstances. His wife said she was able to afford oral nutritional supplementation with Ensure (which she had already been giving him), but I suggested that she add L-arginine. Unfortunately, she said that she could not afford to purchase Juven in addition to his other supplements. I contacted my hospital Abbott rep, and she generously donated enough Juven to supply him for the duration of his treatment course which was several months.
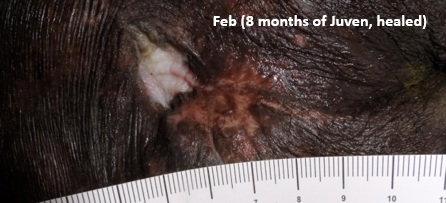
Thanks to the generosity of Abbott, supplementation with Juven began in June. The patient’s wife and I agreed on a reasonable care plan which I told her was palliative in nature. Since it was extremely difficult for him to be transported to the outpatient clinic, I only saw him once a month. By September (3 months later), wound undermining was decreasing. By December (6 months later) there was no undermining at all, and the ulcer was fully granulated with no exposed bone. By the following February, 8 months later, the wound was completely healed.
This patient was dying of a degenerative disease and his calorie intake was insufficient. I had no expectation that a pressure ulcer which exposed the sacrum and was extensively undermined could heal under the best of circumstances, much less under these circumstances. This wound healed, as far as I can tell, primarily because he was taking Juven -since that’s the only thing I really changed about his treatment regimen. Before this experience, I had often recommended L-arginine to my patients, but this case was a turning point for me. I began giving samples of L-arginine to 100% of my patients and spending time educating all of them about its importance. It is now an essential part of every patient’s wound care regimen, which my wonderful nurses help emphasize. We have seen so many other dramatic responses that even before I get into the room of a new consultation, I can hear the nurses telling the patient about the benefits of Juven.



Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



