I am ashamed of how many years it took for me to get serious about the impact of nutritional deficits in chronic wounds, about consistently performing nutritional screening, and about improving patient nutritional status.
There are 3 main barriers:
- Doctors don’t routinely screen patients for malnutrition (it’s time consuming and we’ve got other priorities).
- Doctors don’t know exactly what supplements to recommend
- It’s hard to explain to patients exactly what they need to order and in what quantities (e.g., “You need 2 packets of this a day, which is 60 per week, but they come 80 to a box, and you have to take it for at least 3 months, so if you do the math, that means you should order… etc, etc, etc.)
I’ve already described how my wound care EHR incorporates real-time clinical suggestions to remind practitioners that they need do to nutritional screening, and how it has incorporated the Nestle Mini Nutritional Assessment to make assessment fast and easy. That fixes Barrier #1. What about Barrier #2?
Doctors don’t know exactly what supplements to recommend
It would be wonderful if all the patients could see a registered dietician, but since most of them do not have diabetes, insurance doesn’t pay for that. I had to figure out what to do with the score from the MNA.
I asked for help from Nestle and got it! They helped me develop an algorithm to recommend specific supplements for each of these categories. Every patient with a wound is recommended to have Arginaid (which provides L-arginine, among other nutrients).
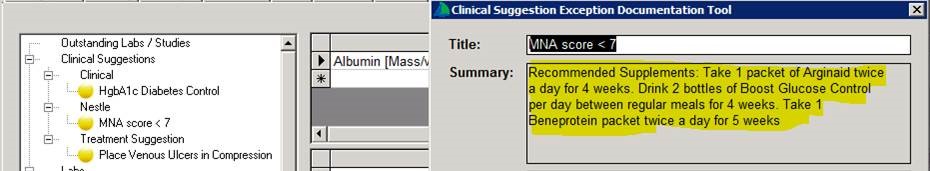
We took this a bit farther, however, and the wound care EHR actually automates the appropriate recommendation through a clinical quality measure tool. I don’t have to try to figure out what I am supposed to recommend for an MNA of 7, for example (which means that the patient is malnourished). In the example above, the patient is a diabetic, and the embedded recommendations actually take into account that the patient needs a diabetes-friendly oral nutritional supplement (ONS) as well as additional protein. (And note, there’s a reminder under Clinical Suggestions that I haven’t performed or documented compression for the patient’s venous leg ulcer).

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.