I have an entire clinic full of patients with pyoderma gangrenosum. Nearly all of them were missed at other wound centers. I am going to post a series of PG cases in hopes that the information will help clinicians and patients identify this disease which is not so much uncommon as “uncommonly diagnosed.” The most important thing I can say is do not trust a negative biopsy.
The first case is an 82 yo woman with a 3-month history of an excruciatingly painful, non-healing left medial ankle ulcer that began after minor trauma from wearing rubber boots. She has diabetes and is overweight. She’s had lesions like this before that started with minor trauma and were hard to heal, not responding to cellular products. She has not responded to compression at another center.
The first question to answer is whether it could be due to arterial disease since she has risk factors for this. Skin perfusion pressure at the ankle was reasonable and her pulse volume recording was normal indicating that arterial disease was not the reason for her failure to heel.
I have found biopsies to be useful less than 50% of the time in cases with chronic, indolent ulcerations and although I usually do them, I didn’t this time. I felt the history of pathergy, the absence of arterial disease, her lack of response to compression, and the appearance of the lesion were consistent with pyoderma gangrenosum. We agreed to a brief trial of prednisone. I actually use prednisone as a diagnostic tool in these lesions because if it works, it makes things better quickly.
After taking only 4 days of prednisone (I picked a relatively low dose due to her diabetes – 20 mg per day) she had a dramatic improvement in pain and the appearance of the wound was significantly better with the development of granulation tissue.
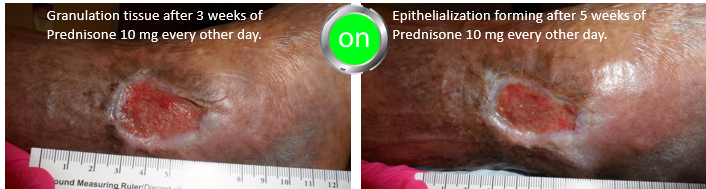
Prednisone was stopped after one week out of concern for her diabetes management and she underwent an intralesional steroid injection but although these often work for solitary lesions, it didn’t this time. The wound was clearly worse after 4 weeks and the pain was back, so she was treated with another week of oral prednisone. I tried to transition her to Dapsone after confirming that she had a normal G-6-PD level, but she had severe side effects from Dapsone. I made the decision to give her 10 mg of Prednisone every other day since she was responding to relatively low doses. Note that by using prednisone every other day, she won’t have to be weaned over a long period of time. She’s checking her blood sugar faithfully.
I put in red the parts of the history that ought to have helped make the diagnosis (a history of pathergy, a prior history of painful lesions, pain out of proportion to the appearance of the lesion, lack of response to appropriate interventions, and no other reason for the lesion). You can see in the photos below the way that the wound improves every time she is on prednisone.





Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




Once the patient heals, do you stop the prednisone or do you keep it for X number of months? I remember a talk by Dr. Ortega and he said that he would keep patients on biologics for maybe up to a year after the wound has healed. I am not sure if that is the same for prednisone. I started a patient on prednisone 20 mg last week and she is also have amazing results. she has not history of diabetes, so I am wondering how long I can keep her on 20 mg daily or when to decrease her to 10 mg every other day.
Hi, sorry if this is a duplicate post.
Once the patient heals, do you stop the prednisone or do you keep it for X number of months? I remember a talk by Dr. Ortega and he said that he would keep patients on biologics for maybe up to a year after the wound has healed. I am not sure if that is the same for prednisone. I started a patient on prednisone 20 mg last week and she is also have amazing results. she has not history of diabetes, so I am wondering how long I can keep her on 20 mg daily or when to decrease her to 10 mg every other day.