I am not a dermatologist and don’t pretend to be one. But, I have seen more pyoderma grangrenosum (PG) than most dermatologists – and so has every wound care practitioner who is paying attention. We all know that biopsies are practically useless, but it is astounding how often even so-called experts rely on a negative biopsy in the face of what seems an OBVIOUS case of PG and refuse to put the patient on steroids even as a trial! The history and clinical presentation are usually sufficient.
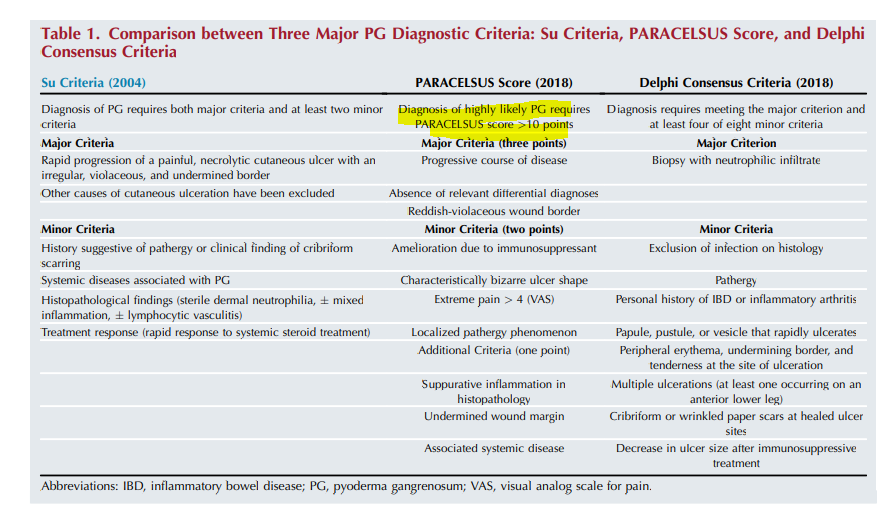
Now there’s a better way. I won’t do justice to the careful work done by Dr. Alex Ortega who is leading the core outcome set group for clinical trials in PG: Understanding Pyoderma Gangrenosum, Review and Analysis of Disease Effects (UPGRADE) (cs-cousin.org). However, I can provide a summary useful for wound care practitioners. The group of experts compared the reliability of 3 different assessment tools with actual cases of PG and determined that the PARACELSUS score was the most accurate (the other two scoring tools were a Delphi tool and the Su criteria). All are very easy to implement but I am going to focus on the PARACELSUS because it may be the best. Note that a biopsy showing “suppurative inflammation”) is good for ONE point. The PARACELSUS score: a novel diagnostic tool for pyoderma gangrenosum – Jockenhöfer – 2019 – British Journal of Dermatology – Wiley Online Library.
As a reference, I am providing the following photos. You will have to trust me that all these patients had PG and they all responded to immune suppression (with prednisone, Dapsone and other agents). Clinical history is useful but you can tell some of it just looking at the photos. One started as pressure ulcer, two of them are post surgical (breast reconstruction and C-section), both on the anterior shin as minor trauma, . In other words, all of them exhibited pathergy. (Most of the time I make the diagnosis of pathergy because the patient is getting progressively worse at a wound center where the doctor is debriding them despite their screams of pain and ignoring their worsening status.) I have attached a PARACELSUS score to each of the photos. I hasten to add that only one of them had a compelling biopsy for PG. Remember that a score of 10 is enough to make the diagnosis. You might be surprised that the C-section post surgical wound has the highest score even though its photo is not as dramatic.
A biopsy is useful to rule out other diagnoses, but not useful to decide whether you are going to initiate a trial of steroids or some other immune suppressing drug. Because all the cases below responded to steroids, they got 2 points. However, if I’d used the PARACELSUS score before I tried steroids, all of these cases would have had a score of at least 10- which is enough to start a trial of immune suppression. Maybe you can use this tool as a way to get support for a trial of steroids among the patient’s other physicians (who have less experience with PG than you do).
Let me know how it goes!
–Caroline
PARACELSUS score:
Major criteria (3 points for any of the criteria below):
- Progressive course of disease
- Absence of relevant differential diagnosis
- Reddish-violaceous wound border
Minor criteria (2 points for any of the criteria below):
- Amelioration due to immunosupessant
- Characteristically bizarre ulcer shape
- Extreme pain (>4)
- Localized pathergy
Additional Criteria (1 point for any of the criteria below)
- Supperative inflammation in histopathology
- Undermined wound margin
- Associated systemic disease






Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.