I have talked about this issue before, but now that the new LCDs governing Cellular and/or Tissue-Based Products (CTPs/skin subs) have been withdrawn (and while we wait to see what the MACs and CMS will do next), maybe it’s worth bringing up again. The use of CTPs has increased eight-fold (based on Medicare claims) in a short period of time, and this equates to billions of additional dollars being spent on them. Most of that increased use is in the private physician office and not the hospital-based wound center, because the payment for CTPs is more favorable in the private office. CMS assumes that this massive increase in spending represents overuse or improper use — and despite all the hand wringing, we have no way to prove otherwise. The tools CMS has at its disposal are blunt. All they can do is reduce payment or limit utilization and unless we come up with a better idea, that’s what they will do.
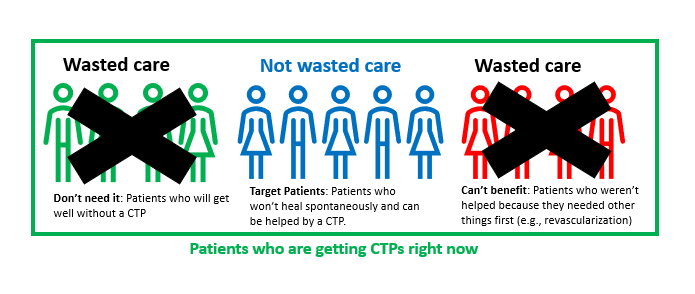
While most of us want to do the right thing for patients and even believe we are doing the right thing, it’s fair to assume that not every physician using CTPs is motivated by altruism. I am going to assume that the current use of CTPs represents at least 3 types of wounds/patients: 1) those who don’t need a CTP or advanced therapeutic (AT) because they are going to get well anyway, 2) the target population of patients who will NOT heal spontaneously but who can benefit from a CTP (because they have adequate arterial supply and good nutrition, for example), and 3) the patients who can’t benefit because their wounds are too severe or they haven’t had the necessary basic care like revascularization.
I have no idea what percentage of current CTP use falls into each of these 3 categories. I would be happy to get your thoughts on what percent of CTP patients fall into each of these categories.
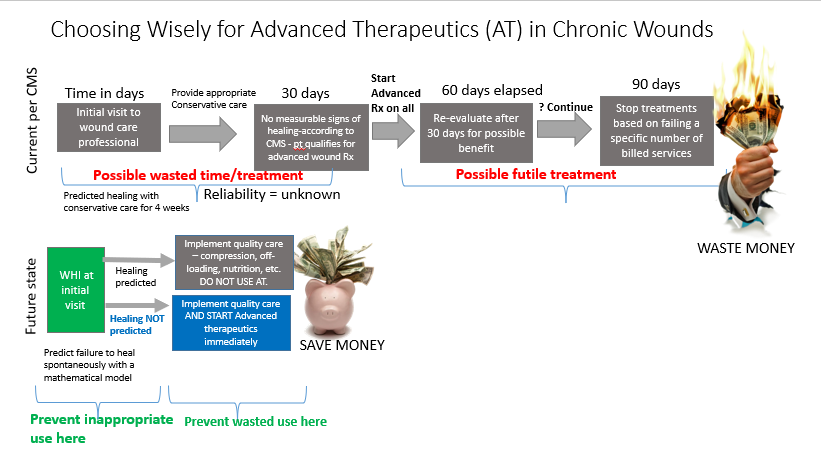
Many years ago, I published a paper in Plastic and Reconstructive Surgery explaining the way that predictive models could be used to better allocate hyperbaric oxygen therapy (HBOT) in diabetic foot ulcers. There was exactly zero interest in this concept for obvious reasons. Making effort to find the patients who need any therapy means NOT providing therapy to the patients who do NOT need it. However, reducing use of HBOT reduces physician and hospital revenue. However, if the alternative to finding the right patients for an advanced therapeutic is that no patients will have access to it – maybe it’s time to talk about how we can choose wisely for CTPs.
Using hyperbaric oxygen as a cautionary tale, in 2000 when CMS approved coverage for Wagner 3 diabetic foot ulcers, as I walked out of the meeting with the CMS Director of Coverage Policy, he said, “We will be watching.” Despite pleas for responsible and appropriate use of HBOT, there was overuse and misuse, and in 2023, the use of HBOT is at a 16-year low and still falling. How did that happen? CMS implemented a prior authorization project in 3 states and launched an audit tsunami that continues to this day. HBOT is current a focus of RAC (Recover Audit Contractors) and every one of the other alphabet soup of audits. Twenty-three years after CMS approved HBOT in DFUs, it’s hard to get HBOT for the patients who really need it.
CMS is going to contain the runaway spending on CTPs. Don’t bother telling me that they are cheaper than an amputation. That argument only works if the patient was at risk for an amputation. CTPs might decrease the total cost of care for a specific ulcer by decreasing time in service or hospitalization. Thus, there may be some patients in whom $100,000 in CTP/skin sub charges actually reduces overall spending. However, for any given patient, there’s a point at which the cost of CTPs cannot be justified from a health economic standpoint. And why do we have to spend $100,000 on CTPs if spending $5,000 on a nearly identical product would work just as well?
We could figure this out if we wanted to, but right now there’s so much money to be made that it’s an uphill battle. We would have to identify the patients who really need them and not treat the ones that don’t need them (we’d have to analyze data to do that). And, we’d have to “do the right thing” consistently when it comes to meeting the standard of care. It’s a lot of work for the practitioner to “choose wisely,” and it’s a lost cause when doctors providing the highest quality care get paid less than the doctors who aren’t adhering to best practices. The quality payment program does nothing to improve the quality of patients with wounds. I do not see manufacturers supporting these ideas, or the clinicians being willing to implement them. We will dither until CMS and the MACS figure out how to turn off the payment tap.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.