I am posting a series of articles with information directly from the websites of the various MACs. Anyone can access this information so I feel a little silly posting it, but several clinicians have told me about audits they are undergoing and they had not paid attention to the type of audit (e.g., Targeted Probe and Educate – TPE, UPIC, etc.), and did not know they could go to the website of their MAC to see what information was available that might help them.
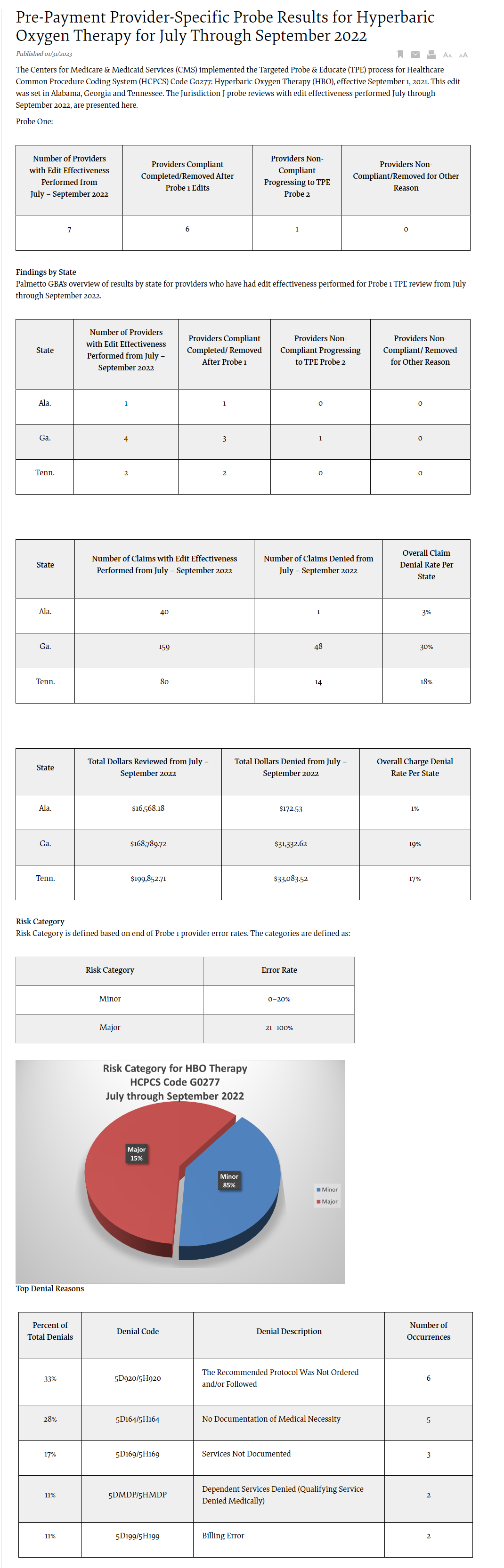
Here’s more information from Palmetto about the Targeted Probe and Educate (TPE) audit process from July through September 2022. There is information by state. It would help if we know what a major vs. a minor risk was (and what that even means).
Palmetto is the MAC for:
- Region J: Alabama, Georgia, Tennessee (Region J)
- Region M: North Carolina, South Carolina, Virginia, West Virginia (excludes Part B for the counties of Arlington and Fairfax in Virginia and the city of Alexandria in Virginia)
- Home Health and Hospice for: Alabama, Arkansas, Florida, Georgia, Illinois, Indiana, Kentucky, Louisiana, Mississippi, New Mexico, North Carolina, Ohio, Oklahoma, South Carolina, Tennessee, and Texas
Denial Reasons and Prevention Recommendations
5D920/5H920 — The Recommended Protocol Was Not Ordered and/or Followed
Reason for Denial
Medicare cannot pay for this service because one or more requirements for coverage were not met.
How to Avoid This Denial
Documentation that may be helpful to avoid future denials for this reason may include, but are not limited to, the following:
For Drugs and Biologicals
- Clear physician’s order with indication of need, dose, frequency, administration time and route
- Date and time of associated chemotherapy, as applicable
- Relevant medical history documented prior to the date of service (DOS) and signed by the physician or appropriate nonphysician practitioner (NPP) to include, but not limited to:
- Clear indication of the diagnosis and need for the related service(s)
- Clinical signs and symptoms
- Prior treatment and response, as applicable
- Stage of treatment, as applicable
- Documentation of administration and signed by the person providing the service
- Ensure the service was provided per the coverage guidelines for the service
For Outpatient Therapy
- Clear physician’s order with indication of specific skilled service, frequency and duration
- Relevant medical history documented prior to the DOS and signed by the physician or appropriate nonphysician provider to include, but not limited to:
- Clear indication of the diagnosis and need for the related therapy services
- Documentation related to the therapy services to include beneficiary’s functional level, treatment plan, short-and long-term goals, beneficiary’s response to therapy services, treatment and progress notes
- Prior treatment and response as applicable
- Ensure the service was provided per the coverage guidelines for the service
For IMRT
- Clear physician/radiation oncologist orders for radiation treatment course, including specific anatomical target volumes, treatment technique, current dosage, type of radiation measuring and monitoring devices to be used and treatment fields
- Relevant medical history documented prior to the DOS and signed by the physician or radiation oncologist or appropriate nonphysician provider to include:
- Clear indication of the diagnosis being treated and medical necessity of the services
- Supporting reports such as dosimetry, physicist, simulation, oncology and radiology
- Documentation of design and construction of multileaf collimator
- Detailed itemized bill and supporting documentation of all billed services
- Documentation of treatment plan, including goals, treatment notes, specific dose constraints for the target and administration
- Ensure the service was provided per the coverage guidelines for the service
More Information
- CMS.gov: Internet Only Manual (IOM), Pub. 100-02, Medicare Benefit Policy Manual, Chapter 15, Sections 50, 220, 230 (PDF)
- CMS.gov: IOM, Pub. 100-04, Medicare Claims Processing Manual, Chapter 4, Section 200.3.1 (PDF)
- CMS.gov: IOM, Pub. 100-04, Medicare Claims Processing Manual, Chapter 17 (PDF)
5D164/5H164 — No Documentation of Medical Necessity
Reason for Denial
This claim was denied because the documentation submitted does not support the medical necessity of the service reviewed. The records did not contain any covered condition/indication, symptomology or diagnostic results that would support the service was reasonable and necessary for the treatment of the beneficiary.
How to Avoid This Denial
- Submit all documentation related to the services billed which support the medical necessity of the services. Documentation should support:
- A covered indication or condition for the service billed
- A physician/NPP is managing the care of the covered indication or condition
- Any medical history that supports a need for the service
- Any diagnostic results or symptomology that supports a need for the service
- A legible physician or NPP signature is required on all documentation necessary to support medical necessity
- Use the most appropriate ICD-10-CM codes to identify the beneficiary’s medical diagnosis
More Information
- 42 CFR — Section 411.15
- Social Security Act (SSA) — Section 1862(a)(1)(A)
- CMS.gov: IOM, Pub. 100-8, Medicare Program Integrity Manual, Chapter 3, Section 3.3.2.4 — Signature Requirements (PDF)
- CMS.gov: Medicare Learning Network (MLN) Matters Number MM6698: Signature Guidelines for Medical Review Purposes (PDF)
- Palmettogba.com — Medicare Medical Records: Signature Requirements Acceptable and Unacceptable Practices
5D169/5H169 — Services Not Documented
Reason for Denial
This claim was partially or fully denied because the provider billed for services/items not documented in the medical record submitted.
How to Avoid This Denial
- Submit all documentation related to the services billed
- Ensure that results submitted are for the date of service billed, the correct beneficiary and the specific service billed
- Ensure that the documentation is complete with proper authentication and the signature is legible
More Information: 42 CFR – Section 410.32, Section 424.5.
DMDP/5HMDP – Dependent Services Denied (Qualifying Service Denied Medically)
Reason for Denial
The dependent services will not be covered if the qualifying service has been denied. For example, the service was denied as documentation did not support medical necessity; therefore, all other charges associated with the service under review cannot be allowed and will be denied as dependent to the medical denial of the qualifying service.
How to Avoid This Denial
- Ensure the documentation provided supports the services were reasonable and medically necessary for the treatment of the beneficiary
- Ensure all records are properly and legibly signed
- Ensure documentation supports the service(s) was rendered
More Information
D199/5H199 — Billing Error
Reason for Denial
The services billed were not covered because the documentation provided did not support the claim as billed by the provider.
How to Avoid This Denial
- Check all bills for accuracy prior to submitting to Medicare
- Ensure that the documentation submitted, in response to the Additional Documentation Request (ADR), corresponds with the date that the service was rendered, and the dates of service billed
More Information
- CMS.gov: IOM, Pub. 100-04, Medicare Claims Processing Manual, Chapter 4, Sections 200.3.1 and 200.3.2 (PDF)
- CMS.gov: IOM, Pub. 100-04, Medicare Claims Processing Manual, Chapter 23 (PDF)
- CMS.gov: IOM, Pub. 100-08, Medicare Program Integrity Manual, Chapter 3, Section 3.6.2.4 (PDF)
Education
Palmetto GBA offers providers selected for TPE an individualized education session to discuss each claim denial. This is an opportunity to learn how to identify and correct claim errors. A variety of education methods are offered such as webinar sessions, web-based presentations, or teleconferences. Other education methods may also be available. Providers do not have to be selected for TPE to request education. If education is desired, please complete the Education Request Form (PDF).
Next Steps
Providers found to be non-compliant (major risk category/denial rate of 21–100 percent) at the completion of TPE Probe 1 will advance to Probe 2, and providers found to be non-compliant (major risk category/denial rate of 21–100 percent) at the completion of TPE Probe 2 will advance to Probe 3 of TPE after at least 45 days from completing the 1:1 post-probe education call date.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.