Medicare updates compared to inflation chart (Cumulative) (ama-assn.org)
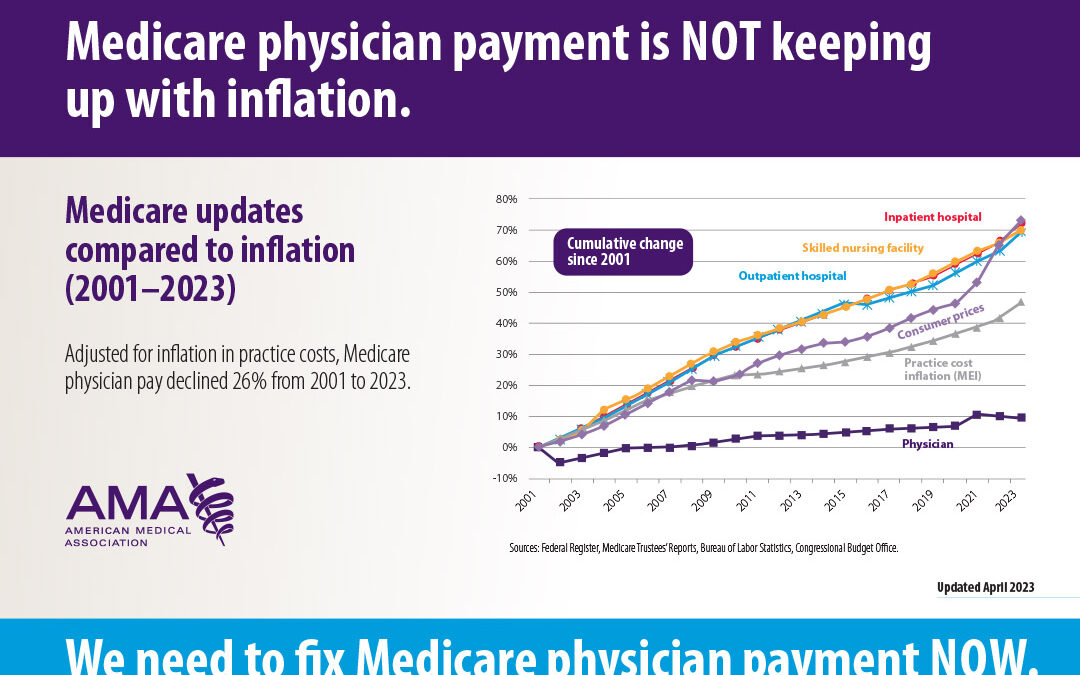
Physicians’ Medicare payments were cut 3.37% on Jan. 1, 2024, on top of a 2% cut that that occurred last year. In total, Medicare physician pay has fallen 26% since 2001 (inflation-adjusted payments) (Figure 1). Meanwhile, hospital payments matched inflation, and over the same period, the consumer price index for physician services in U.S. cities increased by 65%. Many physicians are at a financial breaking point and are either leaving practice or making the difficult decision to stop seeing Medicare patients – or they are finding other ways to make money. It’s understandable.
I personally think this is a factor driving the use of CTPs/skin substitutes in the office-based setting as manufacturers “sell the spread” on these products, and physicians see it an opportunity to make up their losses on Medicare patients. That fuels the vicious cycle of increased Medicare spending, to which CMS and Congress respond with global payment cuts.
Another consequence of the cut is that office-based physicians are paying attention to the Medicare Incentive Payment System (MIPS), now that the COVID-19 exemptions have expired. Physicians who are “eligible” (which is the Medicare term for “required”) to participate based on their patient volume or billed revenue, can see 9% of their Medicare payments cut if they fail to do so. Sadly, in past years, the MIPS bonus payment realized by highest scoring physicians was at best, about 2%. However, in 2024 this “bonus” could at least partially offset the 3.3% cut which occurred on January 1st. Stay tuned for more information about MIPS participation to help survive the 2024 pay cut. I do not have a solution for the CTP/skin sub issue and the downward spiral it creates.
Related Posts:
- How Playing by the Rules with Cellular Tissue-Based Products / Skin Substitutes Can LOSE Money in the Doctor’s Office
- Salve Lucrum: The Existential Threat of Greed in US Healthcare – and Some Thoughts About Cellular Tissue Products (CTP’s) / Skin Substitutes

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.