The story of my son’s intraoperative pressure injuries
In August of 2017, Hurricane Harvey dumped 52 inches of rain on Houston turning the 4th largest city in America into a literal island. However, with our house above water, I was selfishly focused on something else. My 22 year old son had long been scheduled for major maxillofacial surgery to correct a congenital jaw problem, and to my surprise, the hospital called to say his case was still on. I wasn’t too worried because, except for the jaw issue, he’s a completely healthy young man on no medications. That morning we managed to get to the hospital (no easy feat), he walked into the pre-op area and his 5-hour case started a couple of hours later.
To keep my mind occupied during his surgery, I spent the time writing up the case of a Stage 4 buttock pressure ulcer that had developed in the ICU a few months earlier. The evidence was overwhelming that it was a vascular event, specifically, an infarction of the angiosomes that supplied the buttock cheeks. Angiosomes are three dimensional blocks of tissue supplied by a named vessel that typically traverse from the bone to the skin. Plastic surgeons use “maps” of angiosomes to plan flaps for reconstruction, so I was studying the angiosomal maps in the plastic surgical literature while I waited for my son to get out of surgery.
After 5 hours, they brought him to his room with his jaws wired shut which naturally prevented him from talking. In recovery, he’d been handed a clipboard so he could communicate. He showed me the note he wrote in answer to the question, “Are you hurting anywhere?” It read, “MY HEEL HURTS? WHAT DID THEY DO TO MY HEEL?” There were foam dressings over his heels which have become the standard to prevent “pressure injuries.” I had to remove the foam pad over the left heel to inspect it. Under the foam dressing, there was a triangular area of non-blanching erythema on the lateral heel. I started checking the skin on the rest of his body and found a round area of non-blanching erythema over the right lateral malleolus, except unlike the left lateral heel, the right malleolar area was painless.

When the surgeon arrived, I said, “You had to turn him from side to side during the procedure didn’t you?” The surgeon almost laughed. “No, for this surgery, it’s imperative that the patient remain supine the entire time. It’s really important that they not move at all.” I showed the surgeon the pressure injuries on his lateral heel and ankle. “That’s a mystery,” he said. “There were wedges under the back of his ankles, and he was never turned to either side.” After getting my son settled, I sat down to think. What mechanism could be responsible for pressure ulcers on the left lateral heel and right lateral ankle in a healthy patient who was confirmed to have remained supine for a 5-hour operation, and who had walked into the hospital immediately prior to surgery? I’d been writing up that case of the buttock infarction so a textbook illustration of the angiosome map was open on my computer. There was the answer, as plain as the nose on my face.
For 30 years I have been trying to explain “stage 1 pressure ulcers” to myself. It wasn’t what we called them that troubled me — I could not figure out what they WERE. According the available literature, among patients with an intact nervous system, the majority of stage 1 pressure injuries are painful, and furthermore the pain is neuropathic in character. Neuropathic pain simply can’t be explained by local “outside to inside” pressure. Although my son had just undergone a massive maxillofacial operation, it was the excruciating pain in his lateral heel for which he needed morphine. The pain, which had to be coming from the sural nerve, persisted for weeks event though visible changes to the skin resolved in 3 or 4 days. Furthermore, the pattern of erythema was a perfect triangle. There is only one thing that could cause persistent neuropraxia and an area of discoloration with straight borders- and that is something that impacts a vascular territory. See the image below on the distribution of the vascular territory of the calcaneal branch of the posterior tibial artery. The calcaneal branch of the posterior tibial artery emerges laterally between the Achilles and the peroneal tendons. It is easy to understand how the vessel could be compressed within the Achilles.
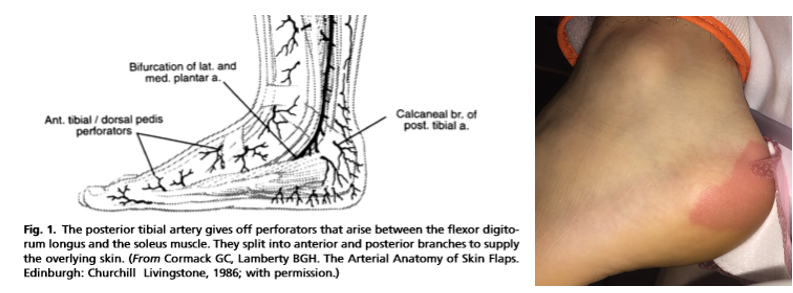
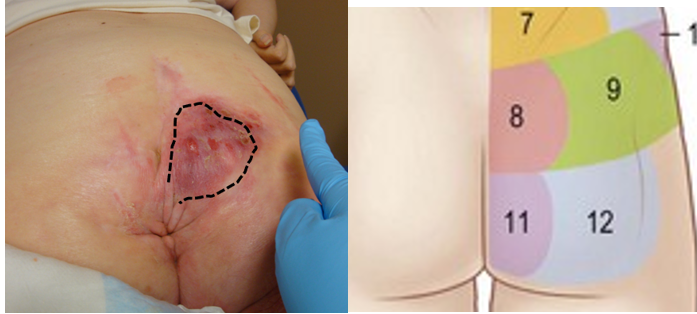
We are all aware of angiosomes thanks to the work of Chris Attinger whose cadaveric studies have revealed these vascular patterns in the extremity. The skin blood supply is divided into anatomical vascular territories defined by the perimeter of the choke arteries which arise from the source vessel. On the extremity they appear as “sectors,” (as they do in the photo of my son) but may follow a neurological dermatome on the torso. Below is a picture of a stage 1 pressure injury on the buttock that follows a dermatomal pattern.
My son had developed an ischemia reperfusion injury to his left lateral heel because the flow to an angiosome had been occluded temporarily, enough to injure the nerve and cause a reactive hyperemia of the area supplied by the vessel. On the left, the affected vessel had to be the lateral calcaneal artery. On the right side, it was the lateral malleolar artery which was affected, because that supplies an annular area right over the lateral malleolus.
With my son’s permission, I reviewed his anesthesia records. It’s typical to keep patients are kept somewhat hypotensive to limit bleeding during facial surgery, but I wondered if his mean arterial pressure had dropped a bit too low. Records showed his vitals were reasonable and amazingly stable throughout the surgery. His hemoglobin was normal post-operatively. There was nothing in his records that would explain the pressure ulcers on his lateral heel and ankle.
 Eight months after the operation, we went to visit Dr. Efthymios Gkotsoulias and tried a little experiment with his very good arterial Doppler and a few colored pens.
Eight months after the operation, we went to visit Dr. Efthymios Gkotsoulias and tried a little experiment with his very good arterial Doppler and a few colored pens.
We re-created the conditions of the operating room with wedges at his Achilles and reported our findings in Advances in Wound Care in an article we called, “On the Origin of Intraoperative Pressure Injury: An Angiosomal Theory of Pressure Injury Formation.”
We used the Doppler to locate the exact position of the lateral calcaneal and lateral malleolar arteries and marked the anatomy on the lower legs with colored markers. Then we simulated his supine positioning in the operating room, placing a wedge at the back of the calf in the Achilles area. In this position, the feet naturally abduct laterally, which places the wedge at the posterior calf exactly at the juncture of the lateral calcaneal and/or the lateral malleolar arteries.

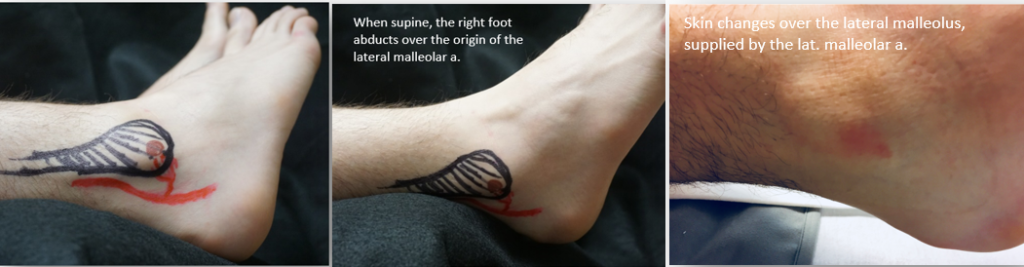
While we can’t prove that the positioning of the wedge is the culprit in the genesis of his pressure ulcers, it is the only explanation that makes logical sense given that direct pressure over the area couldn’t have occurred. We therefore postulate a vascular mechanism of pressure injury development.
And now I finally agree with the term “pressure injury!” There’s no doubt that these Stage 1 pressure events really WERE “injuries” because they were ISCHEMIA REPERFUSION (IR) INJURIES. These Stage 1 pressure injuries most likely resulted from the occlusion of either the arterial outflow or the venous return of angiosomes. An IR injury is also the best explanation for the neuropathic pain that persisted for weeks on the left lateral heel.
This case suggests that at least some heel pressure injuries are NOT the result of localized pressure but rather angiosomal ischemia. We base our theory on the fact that the anatomical pattern of Stage 1 pressure “injuries” frequently follow the distribution of a named vessel. We hypothesize that in this case, intraoperative positioning combined with mild permissive hypotension may have occluded blood flow to the relevant angiosomes, causing an ischemia reperfusion injury to the downstream tissues.
This little observation has big implications:
- If we are right about the mechanism, then not all pressure ulcers are due to LOCAL pressure
- Foam pads on the heel cannot prevent an ischemia reperfusion injury caused by compression of vessels several centimeters away from the heel. Pads might prevent skin breakdown due to moisture or friction, but not IR injury.
- My hospital spends $500,000 per year on foam pads to prevent heel and buttock pressure ulcers. The hospital system spends nearly $5 million dollars a year on foam pads.
- We need to think of positioning through a new lens which is the anatomical vascular supply to the angiosome of an at-risk area.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




Thank you for this fascinating article!
This opened my eyes regarding pressure ulcers and is extremely valuable!
Thank you for your work Dr. Fife. I often have similar questions about patients sustaining DTI after extensive cardiovascular surgeries.
Excellent great insights
This is fascinating! Too bad it was your son but he has a brilliant advocate mom who figured this one out!!!!
This is a great article.
Great article and proof through “field” research. During my time in vascular surgery reperfusion associated morbidity was a well recognized fact and one that could appear with significant challenges. It is a great point that you make about pressure injury being caused not just by local compression of arterial flow but also by “upstream” issues.
Very informative….will share with OR nurses.
Wow….this is great information. Thank you so much for sharing.
Amazing information. Clues that we often search for over the years with certain wounds that don’t make sense. This makes sense. I hope you are going to publish.
Wow, great article, well written, easy to follow. How long before the pain went away for your son? How did the jaw surgery go? Thank you, Virginia
Eyes Wide Open! Thank you for sharing your inSIGHT into this phenomenon!
Great work, I consider you a cross between Matlock and MacGyver!!! This was a great finding & explanation on why we see stage 1 vs the evolution of deep tissue injuries. It was interesting to map out the blood vessels on your son’s foot looking at angiosomes comparing his injury and explaining the “why”. I am sure he is a healthy individual but our sicker patients do not come close to tolerating 5 hours of pressure. To add to your findings – recently we had a referral from another clinic as the heel wound deteriorated. If they were bed bound you would say they had a stage 3 pressure ulcer/injury, but they were ambulatory. By utilizing angiosomes, we could pinpoint causative factors confirmed by noninvasive tests followed by imaging – arterial problem…. Then I compared our data base of actual heel pressure injuries noting the same locations as our arterial patient.
Totally agree with your findings and typically consider these an ischemic reperfusion type injury explaining the evolution of these problems. Recently, I experienced an ischemic reperfusion injury on my hand making the injured skin appear as a deep tissue injury but with prompt interventions the discoloration & tissue loss was minimized.
Dr. Fife – Thank you so much for addressing this concept. There is a lot of misconception and misinformation out there from sales reps selling the idea that foam dressings will prevent pressure injuries. I am the Director of Wound Managment for a Regional Home Health in North Texas, Oklahoma and Kansas and I see a lot of nurses documenting bordered foam to protect heels from PI.
In my ten years of wound care, I’ve seen several ulcers that are right over the lateral malleolus. We’ve spent a lot of effort with local offloading, often to little or no avail. Perhaps you have successfully explained this phenomenon. Thank you for the insight.