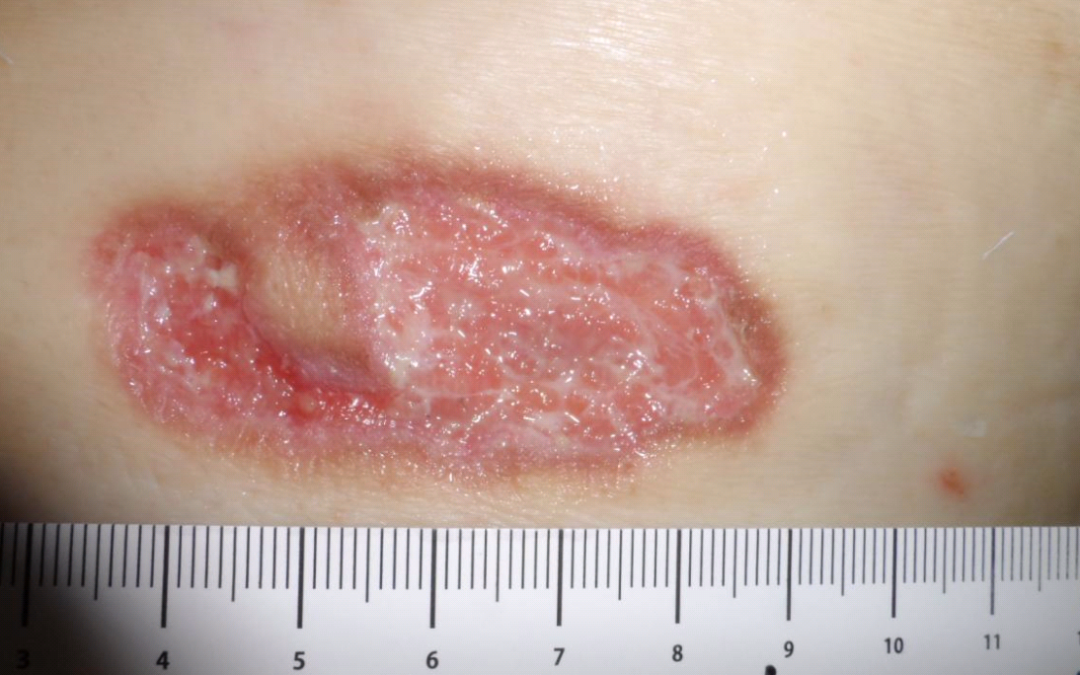
This is a man in his 80’s whose dementia can’t conceal his sweet personality. He has diabetes and relapsing Polychondritis. After he suffered a spiral fracture of the femur due to Myelodysplastic Syndrome, both his surgical incisions broke down a week after surgery. I saw him 2 months later. The first photo shows the strange appearance of the lesion on his lateral thigh. What do you think everyone has been missing for 2 months?

Yes, that’s a smoldering case of Pyoderma Gangrenosum (PG). Remember that this was a surgical incision, so there is no reason for it to have the appearance of an irregularly irregular ulceration. The PG probably wasn’t as aggressive because he’s on Prednisolone for his Myeloma. I could locally inject it with something like Kenalog, but there’s another wound I’m not showing that is very deep and wouldn’t be amenable to injection. I could increase his oral Prednisone, but he has dementia with confusion and diabetes. So, I did something unorthodox that’s been used since the 1950’s- topical Prednisone tablets. It was described in a 1957 issue of the AMA Archives of Dermatology which explained that the “newer compounds” of Prednisone and Prednisolone were synthetic and more potent analogues of Cortisone and Hydrocortisone, and suggesting their use as a topical treatment for various Dermatoses. In a 2014 OWM article, DeMartyn and colleagues described treating Peristomal PG by crushing a 1-mg Prednisone tablet, mixing it with an equal part of a Hydrocolloid powder and sprinkling it directly on the PG lesions, then covering them with a Calcium Alginate dressing.

The Wound at Four Weeks
So, I had the wife crush a couple of Prednisone tablets, sprinkle them into the wound and cover it with a collagen dressing. The other two photos are the wound at 4 weeks, and then when it was healed at 8 weeks. I’ve actually used topical crushed Prednisone several times in PG lesions that are not actively enlarging. It’s cheap, and it doesn’t burn.

Healed at Eight Weeks
I think I’ll post a few other images of PG later because it’s so easy to miss and its presentation is so variable. Think about PG in a painful, irregular ulceration that occurs after trauma whenever a patient has an underlying inflammatory condition.
Sources:
AMA Arch Derm. 1957;76(2):185-188. doi:10.1001/archderm.1957.01550200029006
https://www.ncbi.nlm.nih.gov/pubmed/24905357

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



Hi Caroline, I hope you are well. I suffer from pyoderma gangrenosum and tried this method. I left the dressing on for 3 days. When I took it off, the powder was stuck to the wound. I soaked my ankle in warm water and Epsom salt but there is still residue of the powder and Prednisolone embedded in the wound. It also appears to be slightly worse than what it was before. I’m not quite sure what to do. Any advice?