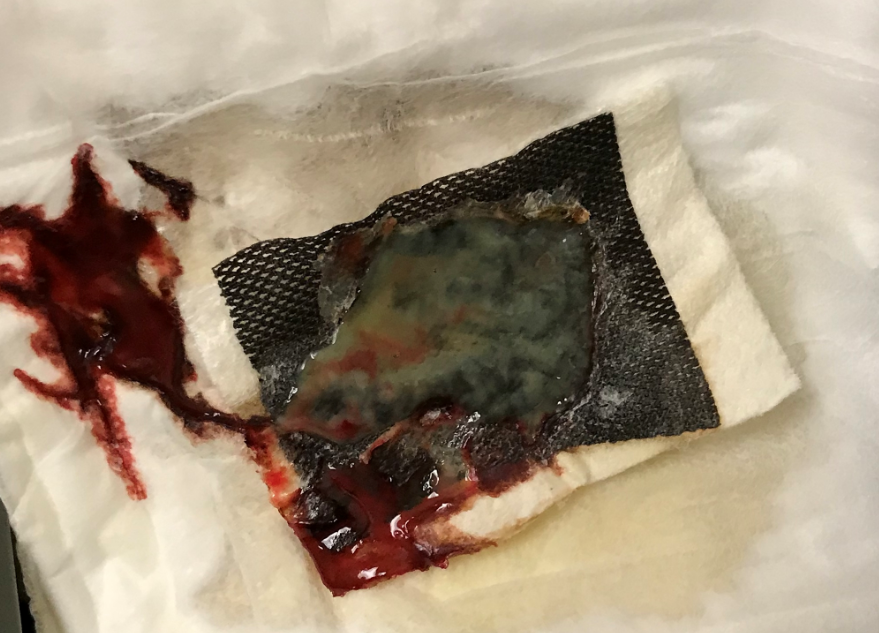
I have the nurses leave the dressing they just removed on a chuck or on top of the trash so that I can look at it. It is amazing what you can learn from a discarded wound dressing. I’ve blogged previously about the fact that frankly bloody drainage is increasingly common. I think it is related to the new anti-coagulants patients are taking. Remember that 24% of wound care patients have atrial fibrillation.
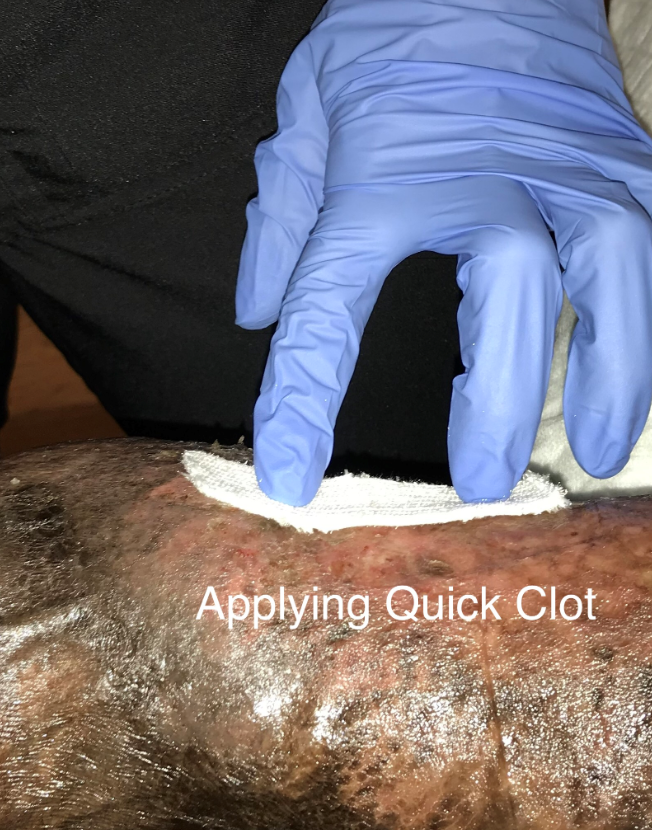
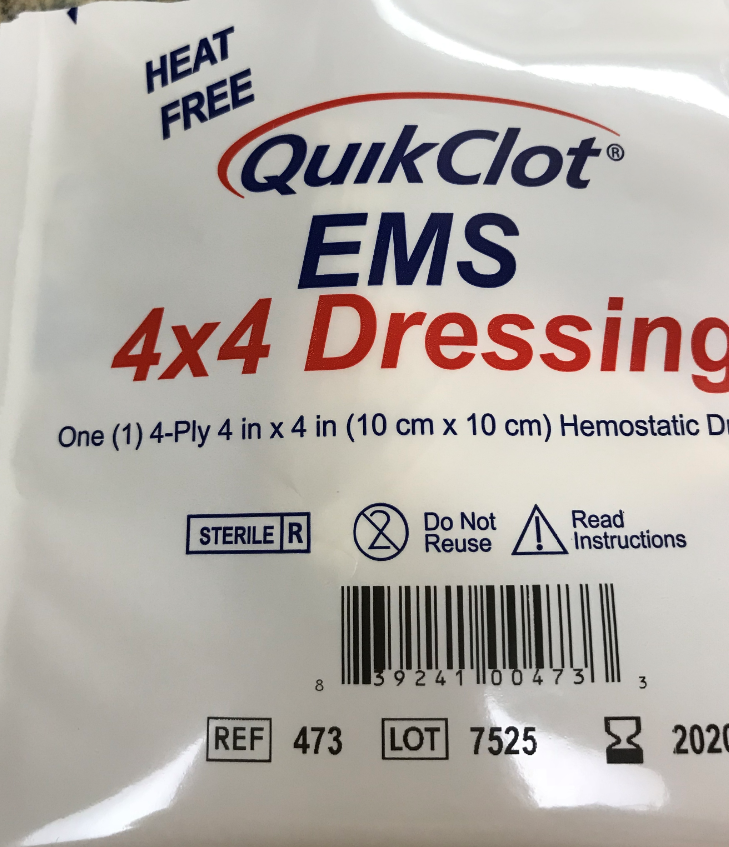
I’d love to analyze the US Wound Registry data to understand the association between bloody drainage and these medications (we have electronic prescribing data and patient medication lists). More importantly, I’d like to understand how bloody drainage impacts healing. Not having hemostasis slows healing down. Lately I’ve been using various Kaolin containing gauze products and it’s making a difference.
I haven’t read an article about this topic – I’m curious if anyone has noticed it. I can tell you that today was a bloody day. I think about 50% of patients had bright red blood in their dressings, including the patients in splints and compression wraps which ought to have limited trauma. I’m suspicious that they are just OOZING, and I think that impacts healing. What do you think?

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.