Last week my editorial in Today’s Wound Clinic stimulated a lot of comment and I was (perhaps rightly) criticized for implying that national wound care meetings are not important. My point is that scientific meetings become a lot less relevant if Wound Management Practitioners are no longer in practice.
I have also been asked why I am the only one who seems to be worried (OK, it’s fair to say I’m panicking). I can’t answer that – did anyone besides me read their Medicare QRUR report or evaluate their MIPS data? Did anyone else read the Federal Register proposed rule on MIPS Value Pathways? Anyone else attending meetings with their Accountable Care Organization or Integrated Network? Anyone logging on to quality websites with private payers to see the quality scores they gave you (which were entirely calculated by them, not based on any data you reported to them?) Is anyone else nominating themselves for the CMS and NQF committees working on episode-based payments (I do know of two other people doing this). I sincerely want to know what people are seeing out there. This is the kind of information tracked by the payment policy professionals in medical specialty societies – which we don’t have in Wound Management. If you have additional insights about these issues – you have an open invitation to guest blog here! I’m stumbling around, but everything I stumble into is bad news.
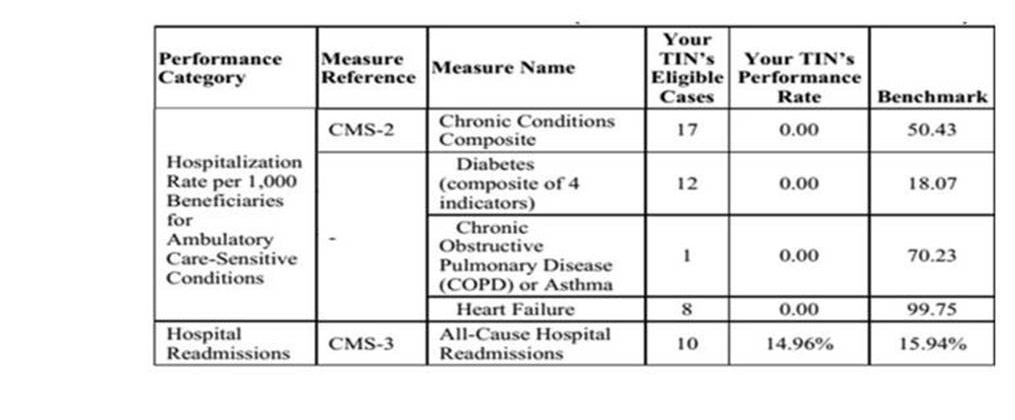
In case you thought I was overreacting, here’s my data showing that CMS holds me responsible for the hospitalization of patients with diabetes, CHF, COPD and heart failure, as well as the rehospitalization rate of most any patient. Medicare thinks I am the PCP because I see these patients more than their other doctors. In 2020 this could affect the physician payment of wound management practitioners as higher percentage of “cost” becomes part of the MIPS calculation:
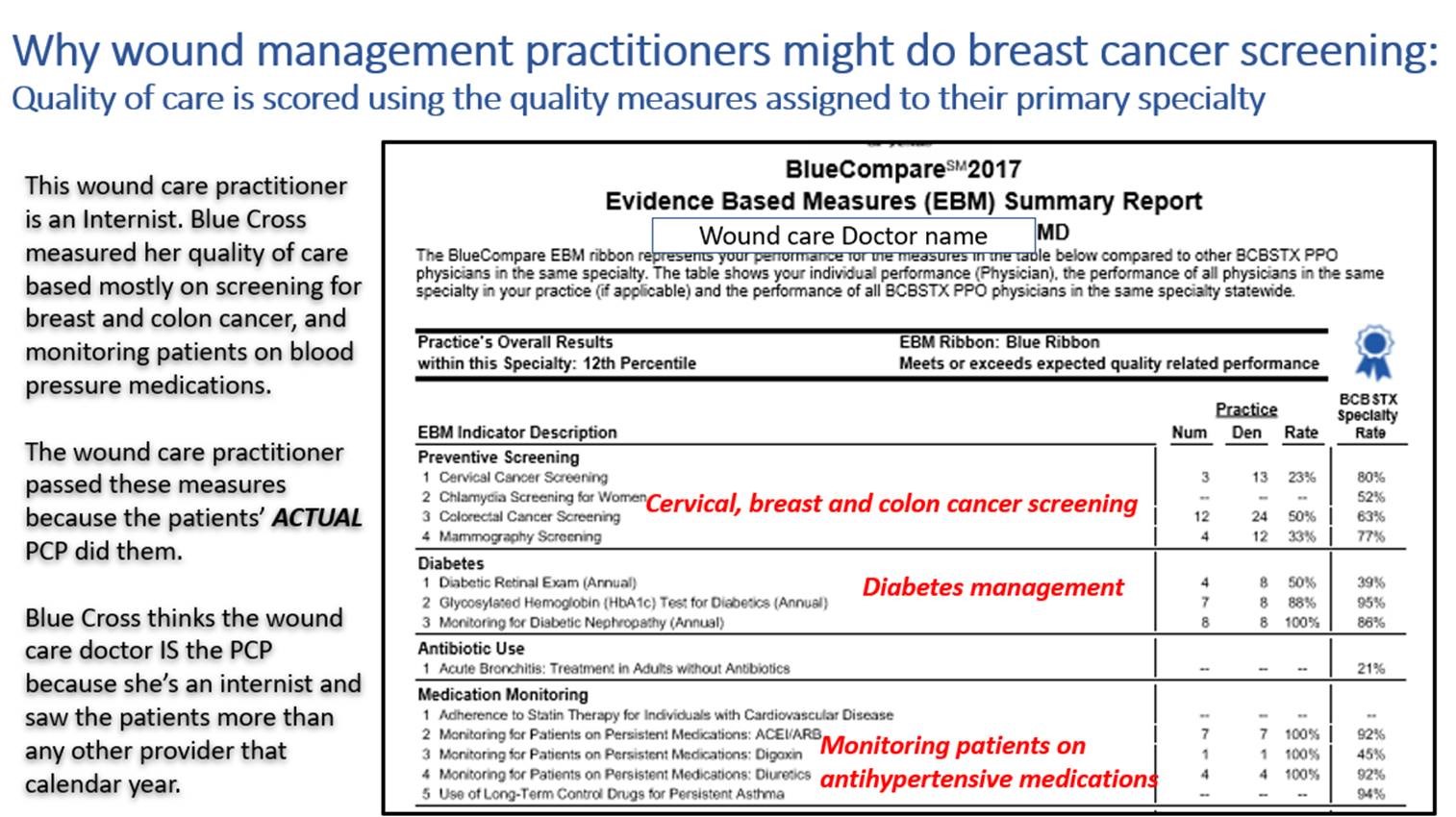
If your primary boards is in surgery or a surgical subspecialty, you will likely survive as wound management physician if you can perform well on the quality measures assigned to your specialty. US Wound Registry data suggest that half of the physicians practicing in wound centers are non-surgeons. They are in trouble. So, to be accurate, perhaps only half of the current wound management practitioners are doomed by their quality and cost report. Here’s proof that this is already being done by private payers like Blue Cross Blue Shield:
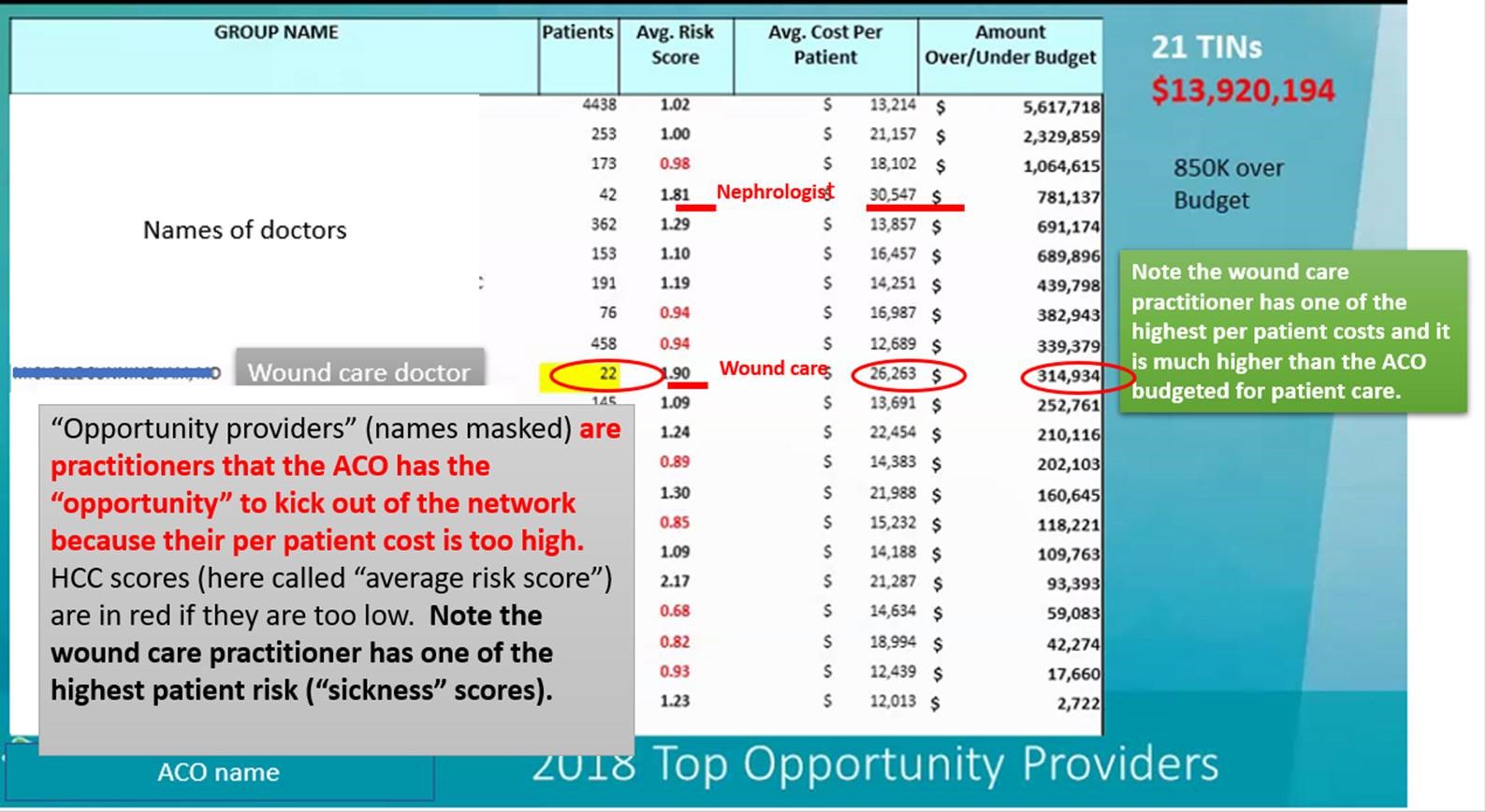
Here’s evidence that Wound Management Practitioners will get kicked out of networks for alternative payment models, because we spend too much per patient compared to peers in our primary specialty:
…and here’s me getting a very nice letter from the National Quality Forum, informing me that I was NOT selected for a committee looking at bundled payment rate for cardiovascular diseases. There are a lot of highly qualified people who apply, often nominated by their specialty society. It’s not the fault of the NQF. Why would they think that a Family Practice doctor would be a good addition to any of these specialty committees?

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.





Caroline it all makes sense, meaning what you wrote, not the inaccurate practice that is going on. How do we (as practicing wound physicians) correct it for ourselves, or panel physicians and for wound care physicians as a whole. I’m a salaried employed physician at this point in my life. I couldn’t get our large group quality department to see the value of utilizing US Wound Registry so we are compared to physicians doing the same job as they felt we (meaning the employed wound physicians) will be diluted by the sheer numbers in our large corporate multi-specialty group. The aren’t going to pay me to attend meetings of CMS or our LCD or any insurance carrier. Truly understand, but who do we petition? How do we do it? and what do you do when you are wrongly tagged with quality measures you aren’t responsible for?
What ever happened to the folks who were intent on forming a “physician only” wound care association of physicians and surgeons who could champion the creation of a new “Wound Care specialist” with board certified status (and thus presumptively a specialty specific CMS acknowledged provider code paired appropriately with the complexity of wound care patients? How do all the CNPs and PTs out there doing wound care look at this issue ? (they come out of non-wound care specialized training programs too).
I can truly understand why you state that you are panicking. In the past year, I have seen almost all of our wound care private practices closing. We closed ours this year, unfortunately in June for the same reason. We are penalized for not doing what we cannot do. Most of the physicians I know are employees of a larger organization. People continue to practice without any real knowledge of wound care . I am not sure what is in the future for my practice. Right now I am struggling to exist, providing care to home bound patients and managing their wounds, being paid almost nothing. There is no benefit to for private practice wound care NP’s at this time.