I’ve talked to a lot of you lately and to save time, I have decided to write an open letter to manufacturers in the wound care space. This advice is free – which means no one will value it, but here is what I wish you were paying attention to:
- Medicare (at least) cares about 2 things: Medicare spending per beneficiary (MSPB) and annual hospitalizations, particularly for cellulitis.
- CMS does not seem to care about healing rates (they know that patients keep getting new wounds) or amputation (which happens infrequently and generally over a time horizon longer than 12 months).
- Last year, CMS rejected the quality measure that reported major amputation rate in leg ulcer patients because it happened “too infrequently” (sic)
- I am mystified why manufacturers do not tie into Medicare claims data to see if their product reduces MSPB or hospitalizations.
- CMS does not seem to care about healing rates (they know that patients keep getting new wounds) or amputation (which happens infrequently and generally over a time horizon longer than 12 months).
- Non-healing Wounds are a SYMPTOM of underlying disease. If wounds were a disease, we’d have a cure by now.
- By way of example, 60% of patients have diabetes, 15% have arterial disease, 20% have atrial fib, 20% have CHF, 10% have end stage renal disease or have had a transplant, and 8% have a collagen vascular disease on prednisone. All of these conditions are excluded in prospective trials (except diabetes in DFU trials).
- If you need examples, check out these blogs, OR COME SPEND THE DAY WITH ME:
- For pity’s sake, the unmet needs in wound care are not VLUs and DFUs. Review the data from the Alliance paper published in Value in Health to better understand the unmet clinical needs in wound healing, at least among Medicare patients:
-
- The most prevalent and most expensive chronic wound is the surgical dehiscence and most aren’t caused by infection (no matter how much CMS blames the hospital) – they are caused by underlying disease
- Surgical dehiscence (particularly on the feet of diabetics) would be a unique niche
-
- For pity’s sake, the unmet need in wound care is GRANULATION. We haven’t had anything new for that since NPWT in 1995.
- Overall, the healing rate of real world wounds is probably less than 50% (certainly lower than we report).
- We COULD report healing rate by predicted likelihood of healing, which would show how well we do in the sickest patients. But so far, the appetite for that is limited because most hospitals just want to say they heal everyone.
- It’s about nutrition. At the very least, collaborate with a company that makes nutritional supplements to incorporate an aggressive nutritional program and as part of your clinical trial, PAY for supplements like L Arginine during your trial.
- We can easily control for standard of care in terms of compression bandaging, DFU off loading, and arterial screening.
- The US Wound Registry QCDR
- Here’s my quality data on Physician Compare (showing that there is national reporting of VLU compression – next year the VLU healing rate measure has been nominated for depiction on Compare). The problem is that you can’t search Compare for the doctors who report this measure. (I have talked to CMS about it but maybe if you talk to them they will listen – I’m an army of one.)
- You need a market reality check on pricing. The HUGE difference in both size of ulcer and number of ulcers per patient has huge implications on how you price your product. For example, most patients have 3 VLUs and their ulcer(s) are 5 times larger than typically enrolled in a VLU trial (see the table below).
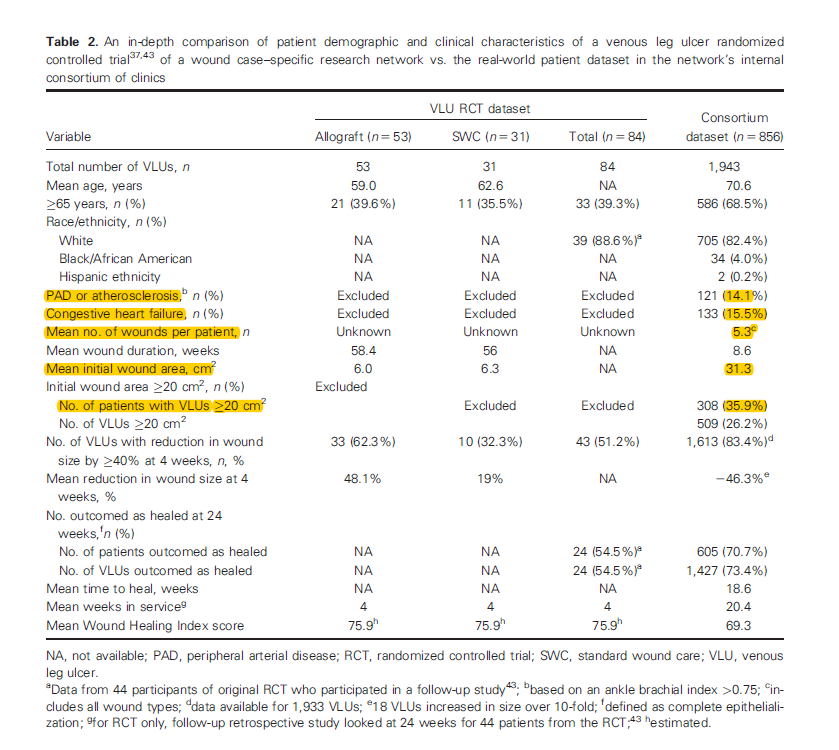
- Almost without exception, cellular product companies perform their trials in wounds we can predict would heal without the product. I understand why you do it, but there are coverage implications.
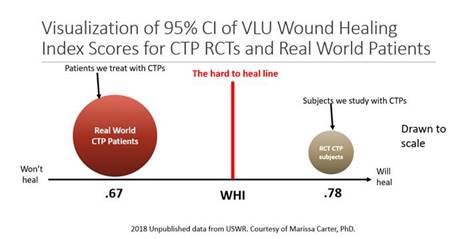
- Below is a Venn diagram created from actual data depicting the VLUs enrolled in nearly all cellular product RCTs with the VLUs seen in the real world. The diagram below shows that the majority of VLUs enrolled in RCTs could have been predicted to heal without them – which means that the trials are designed only to look at the speed of healing and that the trials just needed to run longer. The majority of VLUs treated in the real world would NOT be predicted to heal with conservative care.
- Because we don’t do clinical trials that are relevant to these patients (since the trials exclude all the diseases the patients have), payers refuse to pay for advanced therapeutics because there’s no data to show the interventions help sick patients.
- That means you are about to embark on a multi-million dollar trial to launch a product we won’t be able to use.
- Private payers who administer Medicare Advantage look at the money spent on HBOT, cellular products and other interventions and see only increases in spending without improvements in outcome. Their response is to “just say no.”
- Private payers (and probably Medicare as well) will pay MORE to physicians that can prove they follow evidence-based protocols for care and are willing to submit data to quality registries. For Heaven’s sake, won’t some manufacturer pay attention to this?
We will not be able to use your new product unless you perform more “generalizable” clinical trials. Eventually we will stop getting paid to care for these patients AT ALL unless we stop reporting fantasy healing rates, talk about the fact wounds are a SYMPTOM and not a disease, manage the underlying diseases better, report wound relevant quality measures and go directly to PAYERS to contract higher payment rates for wound care practitioners that can demonstrate high quality care.
I would provide the address where you could mail my check for consulting, but no one pays for advice they don’t want to hear. Good grief no one even listens to advice they do want to hear!

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




This is the best article I’ve ever read. I printed this out and put it on everyone’s desk. Know that Sanara Medtech is listening and we appreciate you!
FANTASTIC!
Was the referenced study performed by Mimedix? If not, please disclose the source. Seems to be a very poor example and certainly isn’t the norm when considering validity of information used in evidence based medicine. I’m very interested in what Manufacture feels this information is even remotely relevant.
Let’s get some real innovation out there!
Exceptional
•”For pity’s sake, the unmet need in wound care is GRANULATION. We haven’t had anything new for that since NPWT in 1995.”
Collagen Induction Therapy and LLLT both need to be researched for GRANULATION.
Thank you Traci!
This is excellent information, you are right, no one will listen…..
Lol! True!
Excellent material! Keep up the hard work of telling us all the things no one wants to hear!
Promise you will sit at the lunch table with me!
Thank you! THIS, All of this, is really why I finally decided to leave Wound Care last year. You have been a voice in the wilderness, Dr. Fife, but the current model just can’t remain viable or defensible much longer. I wish you all the best.
“Thank you! THIS, All of this, is really why I finally decided to leave Wound Care last year. You have been a voice in the wilderness, Dr. Fife, but the current model just can’t remain viable or defensible much longer. I wish you all the best.”
so sad to hear, stay tuned, you might be happy to hear there is a refuge for folks like us…PACE or IHS.
I have a question about supplements and nutrition. If someone did develop an ideal supplement, would any patients actually pay for it and how much would they pay? Would any insurance actually pay for it, even though it might be more beneficial than some super expensive modality? My experience is no.
There was a recent article linking a lack of vitamins C&D, protein, vitamin B12 to amputation rates recently. If the patient’s aren’t getting enough vitamin C, HOW ARE ANY WOUNDS GOING TO BE HEALED?
And, the nutritional problem is more than just wound care.
Maybe the varying government bodies should be focusing on helping patients actually buy REAL food (fruits and vegetables), not just pizza, pop, and boxed foods and then get some education. My wife is an educator in the diabetes space and this is a huge problem. There needs to be more effort towards prevention through nutritional education and lifestyle management so that we can get the proverbial ounce of prevention instead of the pound of cure, which we won’t be able to afford much longer!
Very useful information about wound care products and services. It is great to see your blog thanks for sharing the information.