I was asked to take a look at a 50-page report on a wound center’s post-payment review of hyperbaric oxygen therapy (HBOT) services. Nearly all the wounds that were treated were truly limb-threatening, and most of the patients got better. Unfortunately, their post-payment review has not gone well, and sadly, most of the reasons are avoidable.
I reviewed many (but not all) of the patient records. The issues that I noted largely fall into the categories of:
- Not coding correctly for HBOT to be covered
- Not documenting off-loading of DFU’s at each visit
- Not documenting arterial assessment
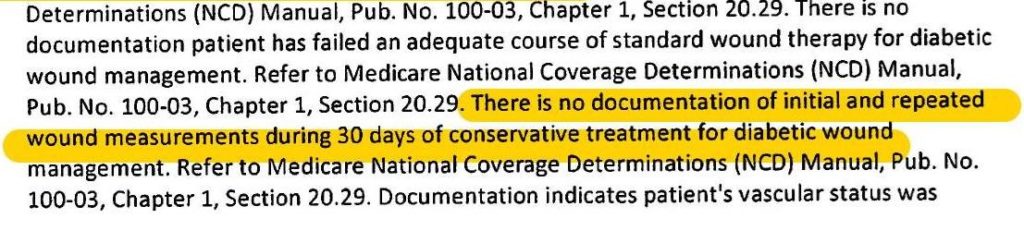
- Not documenting conservative treatments for 30 days before HBOT
- Not documenting studies that would support the diagnosis (e.g. angiograms, MRIs, X-rays, etc.).
Here is some more detail around these issues (see the items in red and my WARNING, below):
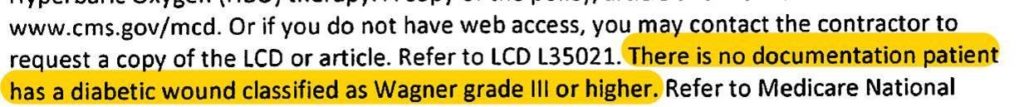
- Wagner 3 DFU not documented: In many cases, the ulcers were clearly a Wagner 3 or 4, but were coded as arterial ulcerations even though the patient had diabetes and my read of the photographs is that the ulcers would better have been coded as DFU’s
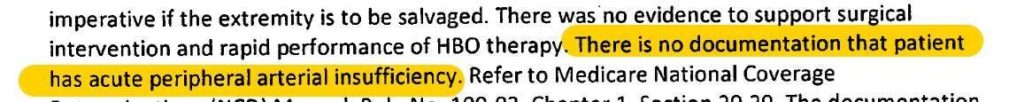
- Needs more clinical evidence to support the diagnosis (e.g. arterial insufficiency)
- The review specifically states that documenting a diagnosis code alone is not enough – there has to be supporting information to prove osteomyelitis, arterial disease, etc.
- No documentation of wound measurements: This one worries me a lot, because I reviewed the clinical records and measurements are clearly THERE. However, I don’t know what was sent to the payer in response to the review. I worry that it might have only been documentation of today’s hyperbaric treatment and not the separate wound documentation.
- No proof of 30 days failed care before HBOT: See concern above in terms of what was sent to the payer.
- No proof of offloading: Off-loading was not documented despite a clinical practice suggestion inside the EHR suggesting that it be documented. In other words, the physicians ignored the tools trying to help them.
- No documentation of arterial evaluation: Every patient should get an arterial screen in the wound center. Pick a modality (ABI, TCOM, SPP, PVR)
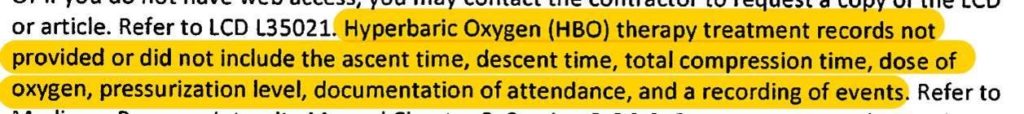
- HBOT records did not include ascent time, descent time, total compression time, dose, pressure, attendance by doctor: ???
- No signed order for HBOT on the date of service
- Record not signed on day of debridement
- Debridement (billed for) was not documented
- Documentation of arterial occlusion but no plan to correct it
- No notes from referring doctor to substantiate neoplasm and prior XRT for late effects of radiation
- No date of skin graft for failing grafts
- HBOT for failing graft was started >30 days after graft
- Too many treatments given for HBOT for failing graft (“not expected to exceed 20” but 30 treatments were ordered and 41 provided)
I highlighted in red some things that have big implications with regard to providing HBOT for a failing graft. The payer is requiring the exact date on which a skin graft was performed, refusing payment if HBOT was started more than 30 days after that date, and refusing payment in excess of 20 treatments.
The payer is requiring that a specific patient with late effects of radiation had notes from the referring doctor to substantiate the diagnosis. That’s big.
A lot of payments are in jeopardy because charts weren’t signed, diagnoses were not coded correctly, or the documentation that was done was NOT SENT in response to the request for records! We can’t survive unless we can do a better job of the basics.
However, a lot of payments are in jeopardy because off-loading was not consistently documented and arterial screening was not done or documented. We have quality measures for those, but no one seems interested in using quality reporting as a way to preserve their payments.
As the Chief Medical Officer of an electronic medical records company with a product specific to wound care, I get asked by a lot of doctors “how long does it take to use your EHR to document a new patient?” They tell me that they are super busy and have a LOT of patients to see and that the EHR will just slow them down. I am sure they are busy. When I am seeing patients I am busy, too. My answer is, “Are you asking me how long it takes to document what you need in order to get paid, or how long it takes to document the way you do it NOW?” Because they are not the same.
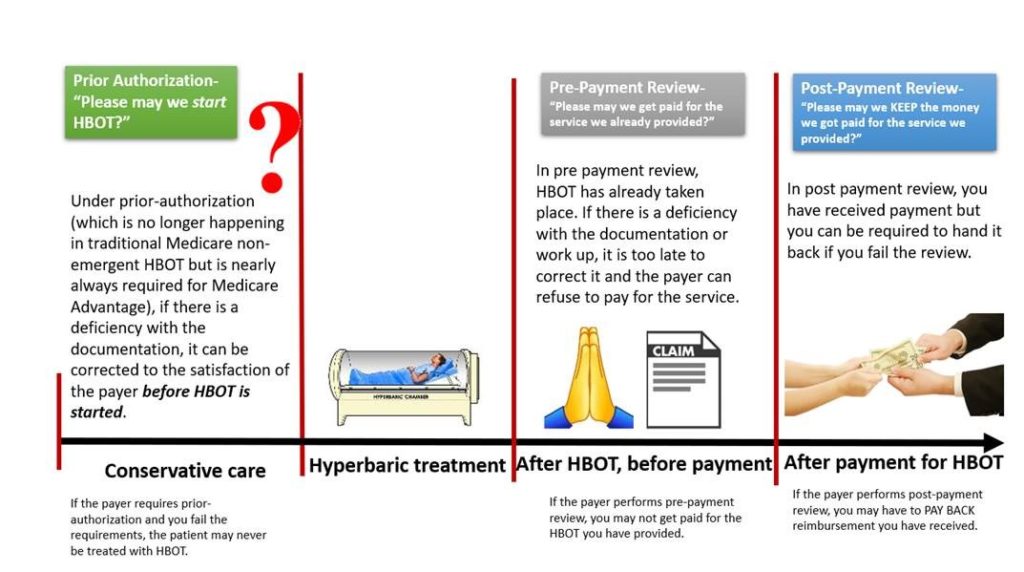
Here’s a graphic to help understand the difference between Prior Authorization, Pre-payment review and Post-payment review:

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



