This interview with one of my patients was filmed one day before my hospital closed to visitors at the onset of the Covid-19 pandemic. The story is so incredible I wanted the patient to tell it herself so I was thrilled when, a few days ago, the Microgen team sent me a link to the finished video. The interview is about how next-generation DNA sequencing saved the life of a patient. When it comes to diagnosing a mysterious disease, I think it’s better than an episode of “House.”
Here’s the Backstory:
For 3 years I have been taking care of a resilient young woman with Type 1 diabetes and a rare autoimmune disease who lost her kidney transplant about a few years ago. She suffers from all the complications of diabetes, and has had many different wound issues. When she returned to see me two years ago, she told me a very odd story. She had been in the hospital twice with sepsis in the preceding 6 months, but the source of her sepsis remained a mystery. All cultures (both bacterial and fungal) were negative. We sorted out her nutritional problems, and I was feeling good about her progress. Then once again, she became septic, presenting with sudden left leg pain, swelling, and the rapidly-ascending erythema characteristic of a necrotizing infection. The transplant team performed fasciotomies of the lower leg and opened her left medial thigh to drain what appeared to be an abscess. But instead of necrotic muscle, the muscle was perfectly pink and only clear, odorless fluid was found, which showed no growth on culture. She was sent back to me as an outpatient to manage her very large post-operative fasciotomy wounds. The surgical team had started Negative Pressure Wound Therapy (NPWT) and we were managing the complex dressing changes in the Wound Clinic.
On one of her fist NPWT changes, I managed to access a persistent fluid pocket in the left thigh. The fluid that poured out was clear and odorless. She was already on intravenous antibiotics, so I sent the fluid for DNA sequencing. (We use MicroGenDx). You can watch this video to understand what DNA sequencing is all about:
The concept is that this polymerase chain reaction (PCR) technique is the most sensitive of the existing methods to detect microbial pathogens in clinical specimens. This is particularly true when the pathogens are hard to culture in vitro. It means that we can find pathogens that used to be darn near impossible to identify. The results have to be evaluated in context with the patient and the situation. It generally takes a few days to receive the final report. Most of the time I am using the information to decide how to treat a complicated list of colonizing bacteria. And to be clear, if a patient has an acute infection, it’s still better to do a traditional culture so you can have antibiotic sensitivities. But remember that all her routine cultures had been unhelpful, and she was already on IV antibiotics. Her wounds looked better with NPWT, but SHE didn’t look better.
A week after I sent the specimen to Microgen, the left thigh wound had grey/black tissue that appeared to be necrotic:


However, unlike necrotic tissue, the dark material could be wiped off with a Q-tip:

In the back of my mind I had this nagging feeling that I had seen this before. The next day, I received the MicroGen report. Here’s the important part of an extensive report:
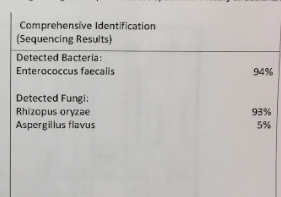
DNA sequencing had detected Rhizopus – also known as Mucormycosis. And then I remembered! I had seen it in about 1992, not long after opening the wound and hyperbaric facility in the Houston Medical Center. Not many immunocompromised patients survive this infection. It’s rare and usually deadly. As soon as I saw that report, I started making urgent phone calls to the patient and to the transplant team.
This is a story with a happy ending. She was quickly admitted to a hospital in the Houston Medical Center where she spent months on intravenous antifungal medication (she continues to take suppressive medications). She also got more surgical debridements, returning to me eventually with even more wounds. But after many months, a few weeks ago, I discharged her with all her wounds healed. And, she’s alive to tell the story. I thought we could all use a happy ending right now.


Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




Incredibly well done!!