We just published an article about the impact of underlying conditions on Quality-of-Life (QOL) measurement among patients with chronic wounds which sheds new light on the use of QOL assessment as well as the underlying medical complexity of these patients. On the face of it, measuring QOL seems like a logical surrogate for wound severity and/or outcome. We all know that having a chronic wound is miserable, thus, it stands to reason that measuring quality of life could indirectly measure the benefit of wound management. If a treatment makes the wound better, that improvement should be reflected in the patient’s quality of life. It’s a logical idea but, it was a big fat failure.
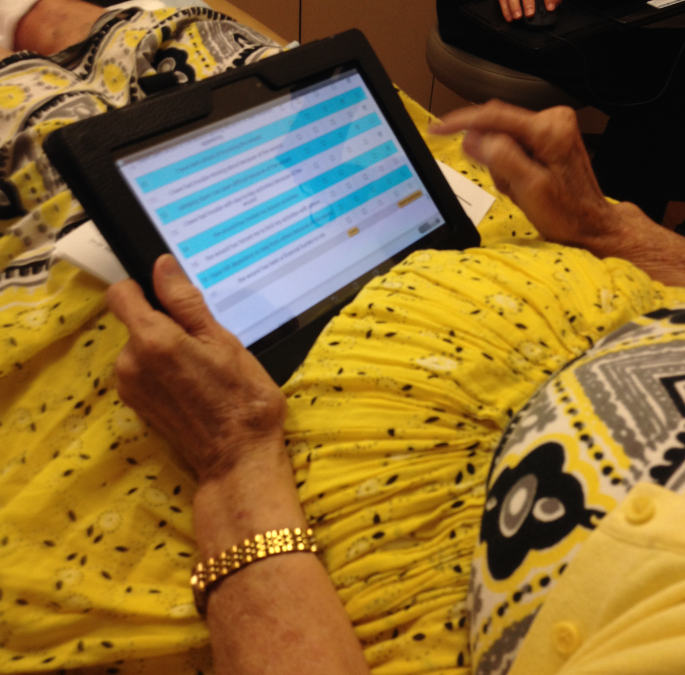
I had great plans for the Wound-Quality-of-Life (W-QoL). In 2015, the U.S. Wound Registry (USWR) got CMS to approve its use as a quality measure that could be reported under Merit Based Incentive Payment (MIPS). The USWR then piloted a project to load the W-QoL on two tablets and administer it to a few hundred patients. The tablet was linked to each day’s schedule, so the nurse could find the patient’s name, give them the tablet so that they answered the questions without influence from the staff, and when the patient was finished, electronically transmit the results to the USWR where they were “married” with the rest of the patients’ registry data on their wound treatment and outcome. The technical part worked beautifully. Here’s a photo of the first patient who used it. She was an elderly lady with terrible arthritis and her only comment was that the low budget tablet we were using in the clinic was not as good as her iPad.
The developers of the W-QoL were thrilled to publish a paper about “validating” the tool based on this pilot study. Validity refers to the extent to which an instrument measures what it was intended to measure. However, just because a tool is “valid” doesn’t mean that it “works.” In this case, the W-QoL did measure quality of life. Unfortunately, the W-QoL failed to show a relationship between the W-QoL score and wound severity or outcome. There are several reasons. A big reason is that almost every chronic wound patient has at least two wounds. It would be necessary to get the patient to specify WHICH wound was the one that they were thinking about when they answered the QOL questions and unfortunately, I didn’t think to specify that when we gave patients the questionnaire. I am not even sure that doing so is possible since the impact of chronic wounds on a patient is cumulative, not separate. Another reason for its failure is that many questions focused on activities that the patients couldn’t do regardless of whether they had a wound, such as climbing stairs.
But the primary reason that the W-QoL failed as a surrogate for wound severity and/or outcome was the severity of the patients’ co-morbid conditions. Among the 382 patients to whom we gave the survey, there was one young man with a pilonidal cyst who had no other health problems. In a 15-year-old with a pilonidal cyst, the W-QoL can probably capture the impact of the wound on his quality of life. However, the rest of the patients had issues like heart failure, autoimmune diseases, or were paralyzed – meaning, they were our usual chronic wound patients –they were very SICK. Although we all say that “our patients are complicated,” no one has ever tried to capture exactly how complicated. That’s what this new publication is about.
We wanted to understand the impact of underlying comorbidities in a real-world patient population, so we examined this convenience sample of 382 patients seen at a hospital-based outpatient wound center. The mean number of comorbid conditions per patient was 8. We then used the concept of “utility values” to better understand exactly how much these underlying diseases affected them. We found that 229 patients (59.9%) had utility values for comorbidities/conditions which were worse/lower than the utility value associated with their wound. Sixty-three (16.5%) patients had depression and/or anxiety, 64 (16.8%) had morbid obesity, and 204 (53.4%) had gait and mobility disorders, all of which could have affected W-QoL scoring. Translation: The patient’s underlying condition had such a powerful impact on their QOL, it wasn’t possible to measure the incremental effect of the wound(s) on QOL.
This study has a lot of implications. The obvious one is that it may be impossible to use typical QOL tools as a surrogate for outcome unless the patients are atypically healthy. Since most prospective, randomized, controlled trials in chronic wounds exclude serious comorbid diseases, quality of life might work in those trials. That’s just another proof of how “non-generalizable” RCTs are. A major implication of this paper is to demonstrate just how sick the average patient with a chronic wound IS. As we keep saying, non-healing wounds are a SYMPTOM of underlying disease. That’s why I don’t think we will ever find the cure for non-healing wounds with a product that is local to the wound. The reason that patients don’t heal is systemic. But I digress… And while I am giving out opinions that have nothing to do with the paper I am talking about, these comorbid diseases may mean that what we CALL the wound doesn’t matter as much as anyone thinks. We could revolutionize clinical trials if they were focused on randomizing patients according to their comorbid conditions rather than some artificially created definition of a wound that is not relevant to the typical patient. Unfortunately, I don’t see anyone funding that study.
By the way, CMS killed the quality measure that focused on measuring quality of life in patients with chronic wounds. Their argument was that simply MEASURING QOL is not a quality activity. CMS expected the QOL to be used to help manage the patients or as a surrogate for outcome. CMS wanted us to show a specific percentage improvement in QOL if we were to use it as a surrogate for outcome. Since the QOL had no relationship to wound severity or outcome, that was never going to happen. What’s also never going to happen is getting the average clinician to measure QOL. It’s time consuming and you can’t get paid for doing it. So, if you are a manufacturer reading this post, the next time you ask me if the USWR has quality of life data on chronic wound patients, stand out of the range of my fingernails. This entire project was entirely unfunded. If manufacturers want QOL information on how their products work, they will have to pay clinicians to collect it. But first, they will have to find one that works.
–Caroline

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.