Guest Blog by Davis Melin and Mark Melin
Gravity humbles the human body. The acute effects of gravity include falls and fractures while the chronic effects include sagging skin that not even Botox can overcome. Because of gravity, fluid in the body naturally falls to the lowest point — usually the feet. To combat this, the lymphatic system must actively work to pump fluid from the feet all the way up to the left subclavian vein in the chest. This is not an easy task under normal circumstances, but it is even harder if there are injuries, volume overload, leaky blood vessels, or genetic abnormalities that affect lymphatic function. Altered lymphatic function can lead to interstitial tissues taking on extra fluid, a condition called lymphedema which is well known to negatively impact wound healing. What is not well known or understood is that lymphatic dysfunction may also be linked to a specific chronic pain syndrome.
New evidence suggests that lymphatic dysfunction may be linked to Chronic Regional Pain Syndrome (CRPS) (1), a debilitating problem poorly responsive to current treatment options. A recently published case report describes a patient with multiple leg fractures who developed compartment syndrome necessitating fasciotomies and who subsequently developed CRPS. Like most patients with CRPS, the pain was poorly responsive to medications, lumbar sympathectomy, exercise therapy and acupuncture. Mysteriously, the patient had also developed chronic leg edema despite the absence of a deep venous thrombosis (DVT) or any evidence of venous insufficiency. Dependency and increasing edema worsened the CRPS pain while edema reduction from compression stockings and leg elevation improved it. The case report describes an improvement in leg pain associated with the use of a new 16 chamber manual lymphatic drainage “mat” that is FDA approved for pain control. In other words, CRPS-related leg pain improved thanks to lymphatic treatment of the back – an area far distant from the lower extremities.
Curiosity brought a group together to address the question, “Why would stimulation of the lymphatics of the back impact lower extremity lymphatic function and improve CRPS pain?” One potential theory was that the mat was stimulating the autonomic nervous system, specifically the sympathetic nervous system. Scientists are learning that the lymphatic system is likely entirely enervated by the “fight or flight” sympathetic side of the autonomic nervous system versus the “rest and digest” parasympathetic side. The lymphatic system and sympathetics communicate through neurotransmitters and neuropeptides to maintain fluid homeostasis. When the lymphatic system is dysfunctional, interstitial fluid builds up along with inflammatory cytokines which increase microvascular permeability, overloading the lymphatic drainage system and causing a vicious cycle that also contributes to pain (2, 3). Therefore, it seemed plausible that improving lymphatic function might improve pain management and provide a new treatment option to individuals with CRPS.
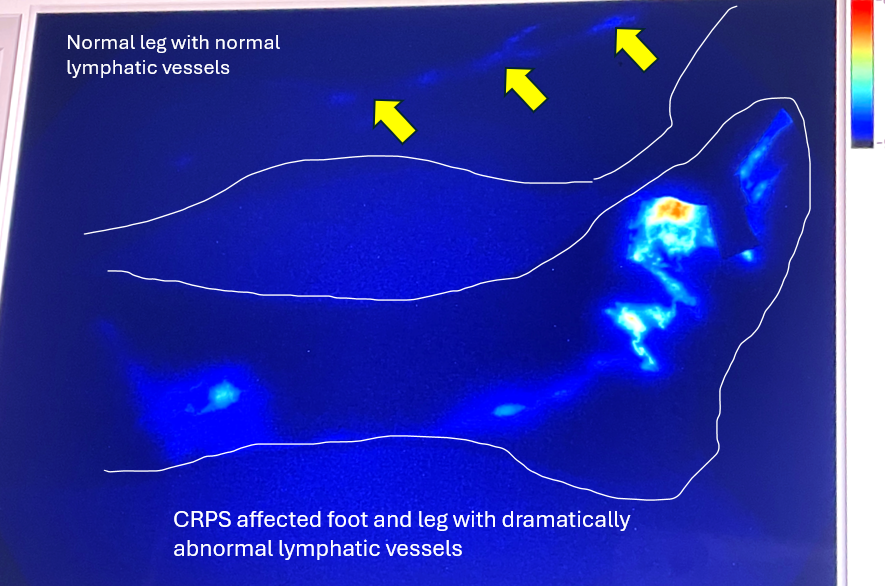
To test this idea, the group used Near InfraRed Fluorescence Imaging (NIRFLI) to observe and measure the rate of lymphangion contractility and pulsatility in response to treatment with the mat(4). The first thing the group noticed in the case of the patient with CRPS was that the lymphatic vessels in the limb were dramatically abnormal (see photo). They were “functional” in that the vessels could contract and move fluid, but everything about their anatomical appearance was abnormal. NIRFLI imaging confirmed that the pneumatic chambers stimulating the subject’s back activated lymphangion pumping – the contractions of the lymphatic segments that move fluid in “packets” through the lymphatic vessels. Check out the videos of the lymphatics.
Although single case reports must be interpreted with caution, these are novel findings. The results support the idea that there is a connection between the lymphatic and autonomic nervous systems and that lymphatic dysfunction is directly related to CRPS pain. The results offer hope to CRPS sufferers. Improving lymphatic function may improve the underlying cause of CRPS and thus improve pain—offering a possible opioid-free pathway for CRPS management. Perhaps a new understanding of the underlying pathophysiology of CRPS includes lymphatic dysfunction and targeting that could help us find better treatments in the near future.
- Melin MM, Rasmussen JC, Aldrich MB, Karni RJ, Fife CE, Eckert KA. Additional evidence from a case report supports a novel hypothesis on the association between complex regional pain syndrome and lymphedema. Front Pain Res (Lausanne). 2025 Jun 26;6:1540930. doi: 10.3389/fpain.2025.1540930. PMID: 40641619; PMCID: PMC12241101.
- Tuckey B, Srbely J, Rigney G, Vythilingam M, Shah J. Impaired lymphatic drainage and interstitial inflammatory stasis in chronic musculoskeletal and idiopathic pain syndromes: exploring a novel mechanism. Front Pain Res. (2021) 2:691740. 10.3389/fpain.2021.691740 .
- Aldrich MB, Sevick-Muraca EM. Cytokines are systemic effectors of lymphatic function in acute inflammation. Cytokine. (2013) 64(1):362–9. 10.1016/j.cyto.2013.05.015
- Aldrich MB, Rasmussen JC, Karni RJ, Fife CE, Aviles F, Eckert KA, et al. Case report: the effect of automated manual lymphatic drainage therapy on lymphatic contractility in 4 distinct cases. Front Med Technol. (2024) 6:1397561. 10.3389/fmedt.2024.1397561
Davis Melin MPH, 4th year Medical Student, Pre-PMR, Liberty University College of Medicine, Lynchburg VA
Mark Melin MD, Gonda Vascular Center, Wound Clinic Medical Director, Mayo Clinic, Rochester, MN
Additional Resources:
- Lymphatic Imaging & Lymphedema – Caroline Fife M.D.
- Near-Infrared Fluorescence Lymphatic Imaging Confirm Changes in Lymphatic Function Before Visible Lymphedema – Caroline Fife M.D.
- Check Out This Paper on the Effect of a New, Automated Manual Lymphatic Drainage Therapy Device – There are Links to Downloadable Videos of the Lymphatics Pumping in Real Time! – Caroline Fife M.D.
- The (Mostly) Complete Guide to Lymphatic Anatomy: A Free Synopsis of Everything We Know Now – Caroline Fife M.D.
- Check Out the Amazing Images of the Lymphatic System in This Review Article! – Caroline Fife M.D.
- New Review Article Just Out: The Development and Treatment of Lymphatic Dysfunction in Cancer Patients & Survivors – Caroline Fife M.D.
- Sea Turtle Fibropapillomatosis: The Role of the Lymphatics (and Why Clinicians Need to Keep Their Eyes Open) – Caroline Fife M.D.
- Lymphatic Function in the Early Stages of Lipedema – Article Just Out! – Caroline Fife M.D.
- Watch This Video of Lymphatic Dysfunction in Venous Disease! – Caroline Fife M.D.
- Lymphatic Dysfunction in Cancer Patients – Insights Into This Mysterious and Vital Organ System – Caroline Fife M.D.
- Why My Blue Mondays are Happy – Caroline Fife M.D.
- If Success and Failure Look the Same Clinically, We Have a Problem – Caroline Fife M.D.
- Axillary Web Syndrome Revealed – Caroline Fife M.D.
- New Study Shows That Even Patients With Early Venous Disease Have a Degradation in Lymphatic Function. Use My Personal Share Link to Obtain a Free Copy! – Caroline Fife M.D.
- Watch “Myths Debunked! How Lymphatic Imaging is Changing Patient Treatment Plans” and Read the Article! – Caroline Fife M.D.

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.



Together we planted the wound / lymphatic seed in 2001- Love the forest we have now!👍
Together we planted the lymphatic / wound healing seed in 2001. Love the forest we see today! 👍