“You can’t fall asleep while I am talking to you unless we are married.” That’s what I say to all the patients who fall asleep in the exam room. It seemed humorous at first, until I realized that sleep apnea could be the reason that some patients were not healing. Sleep apnea might be the reason they had leg edema, were forgetful, and had cardiac issues. What if sleep apnea was the underlying cause for most of the medical problems they had? After all, every patient with severe venous disease does not get a venous leg ulcer, and every diabetic does not get a diabetic foot ulcer. Something else is involved. Perhaps the most important question we can ask patients (other than, “Do your feet hurt?”) is, “Do you sleep in a chair?”
Sleep apnea was a major contributor to my husband’s mental decline and death. If I had known then what I know now – his outcome or at least his clinical course would have been very different. However, my personal experience showed me that when these problems develop slowly, the patient and the family just think it is “normal.” It is not normal.
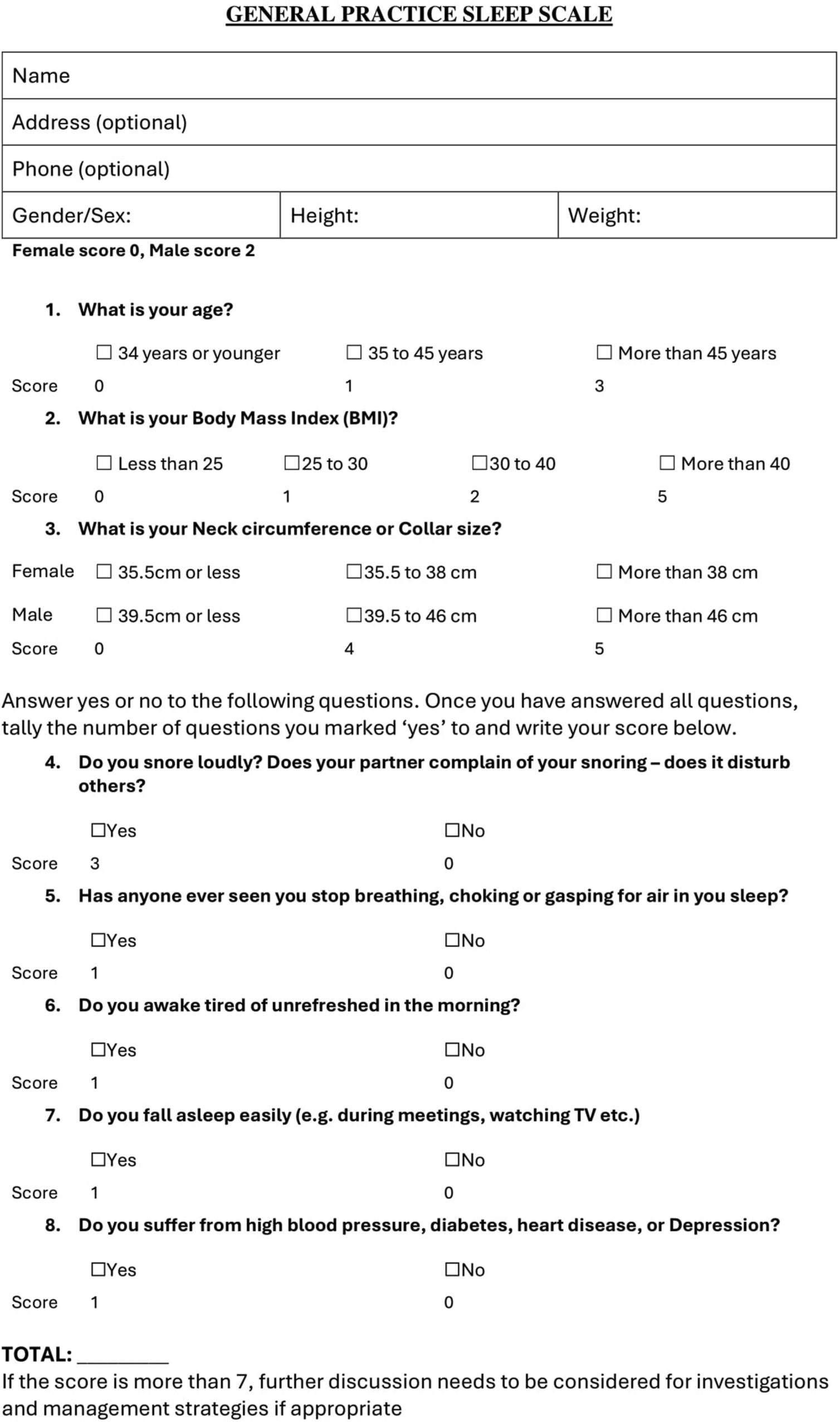
Given the direct connection between OSA and the problems that plague our patients (edema and chronic non-healing wounds) wound care practitioners (who have more time with patients than their primary care doctor) we should screen patients for OSA with the General Practice Sleep Scale (GPSS). It’s fast and easy to do. The scale assigns a score of low, moderate, or high risk of obstructive sleep apnea based on a patient’s responses across nine dimensions.
What if the treatment patients most need is not something that goes on the wound?
Resources:
- General Practice Sleep Scale – The “GPSS” – A proposed new tool for use in General Practice for risk assessment of Obstructive Sleep Apnoea – ScienceDirect
- Vitamin D Deficiency and Pediatric Obstructive Sleep Apnea Severity – Caroline Fife M.D.
- Tirzepatide Improves Sleep Apnea, Based on a New Study Published in NEMJ – Caroline Fife M.D.
- Sleep Disorders an Early Dementia ‘Warning Sign’?

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.