I heard a few firecrackers on New Year’s eve, but the big fireworks in our industry go off on January 7th, 2019. That’s because the Centers for Medicare & Medicaid Services (CMS) has established a new physician specialty code for Undersea and Hyperbaric Medicine (D4), effective January 1, but with an implementation date of January 7, 2019. When a physician enrolls in Medicare, he or she “self-designates” their specialty on the Medicare enrollment application (CMS-855I or CMS-855O) or Internet-based Provider Enrollment, Chain and Ownership System (PECOS). You do not have to be Board-Certified in the specialty you self-designate. For example, for most of the 23 years that I was on the faculty at the University of Texas Health Science Center in Houston, I was in the Department of Anesthesiology. As a result, my department designated me as an anesthesiologist on my PECOS form, even though I am Board-Certified in Family Practice. When I later moved to the Cardiology Division of Internal Medicine, the university changed my specialty designation to Cardiology! When I left the university and went into private practice, I changed my self-designation to Family Practice even though I was practicing Wound Care and Hyperbaric Medicine. Why? Because even though I am actually subspecialty Board Certified in Undersea and Hyperbaric Medicine via Preventive Medicine, there was no way to designate that on the PECOS form.
Specialty codes are used by CMS for programmatic and claims processing purposes. Why does this matter? By using the D4 designation, practitioners can “explain” to CMS the nature of their particular practice. I will give you an example from my 2017 MIPS report. In 2017, Medicare did not include “cost” in the calculation of the MIPS score, but they reported data about cost for each participating physician to see. My 2017 cost data were very interesting. In 2017, CMS calculated my total per capita cost (TPCC) at $24,306 and my per-episode cost at about $58,000. This was CMS’ analysis of how much money was spent on my patients (at least, on the patients with conditions CMS cares about, such as heart failure and diabetes with complications, etc.). After calculating these costs, CMS then compared my cost data with those of other family practice physicians because I self-designated as a Family Practice physician. Not surprisingly, compared to my colleagues in Family Practice, I had a much higher per patient costs. And as a result, CMS assigned me to the 3rd decile (which is actually as bad as you can get). That’s really bad. In other words, CMS told me that I spent too much money per patient compared to other Family Practice doctors. In fact, they said I spend way too much money in general. And, of course I do given that my patients have an average of 10 serious co-morbid conditions and take an average of 12 medications – as Helen Gelly and I showed in our analysis of hyperbaric registry data. In 2017, why didn’t CMS compare my data to other hyperbaric practitioners? Because there was no specialty designation code to enable CMS to know who the other hyperbaric practitioners actually were.
In other words, unless you are a critical care physician or transplant surgeon, your typical hyperbaric patients are likely to be more complicated than the average patient cared for by colleagues in your original specialty. This could result in your receiving a low decile ranking in the cost category of MIPS, a category that is taking on more importance each year. However, if you change your designation to D4 to reflect the fact that you are a hyperbaric medicine practitioner, then CMS will compare your spending with your peers in hyperbaric medicine. Changing your designation to D4 will decrease the chances that you will lose Medicare money because of a poor MIPS cost score. It also allows us to collect accurate data on total per capita charges among hyperbaric patients.
This is another reason I keep blogging about “visualizing” the complex patient and why it’s imperative we report FAILURE TO HEAL rates. CMS knows we have episode costs approaching $60,000 and it ought not to be surprising given that such a large percentage of our patients have congestive heart failure, atrial fibrillation and renal impairment (as only one example of a Medicare “triad” which are guaranteed to cost $60,000 a year). I see at least one patient like that a week!
What if you don’t see a lot of hyperbaric patients but the majority are wound care patients? One of the criteria for the specialty designation was that a specific code or codes existed which defined the scope of practice. That was pretty easy with hyperbaric medicine, but it’s not that easy with wound care since there is overlap by several types of specialists. That means it may be hard to get a wound care subspecialty or specialty designation. In the meantime, the type of patients seen by hyperbaric oxygen therapy practitioners is more like those in chronic wound care than any other group that comes to mind. Remember the purpose of the designation is to convey to CMS the nature of your practice. It is certainly more accurate to say that I practice hyperbaric medicine than Family Practice, even if only a small percentage of my patients actually are treated with HBOT.
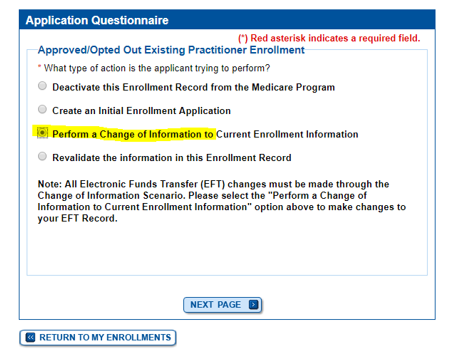
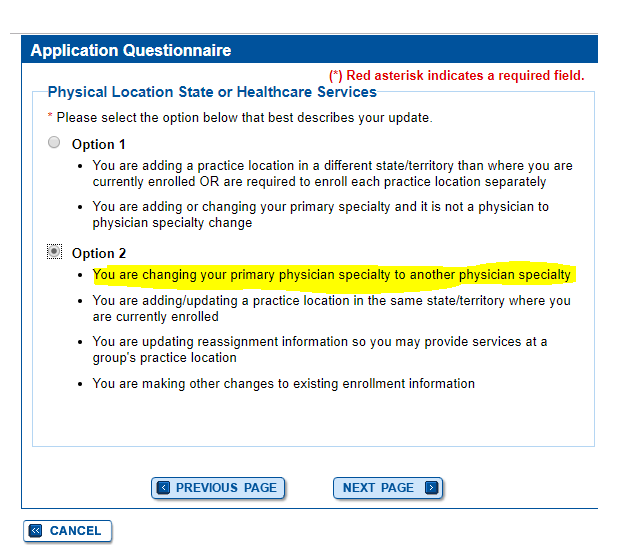
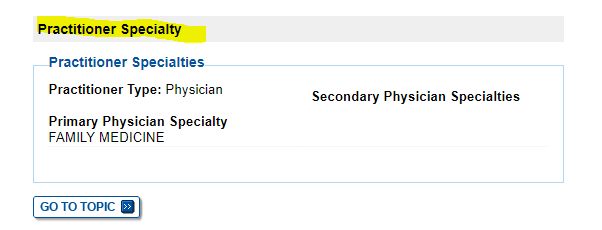
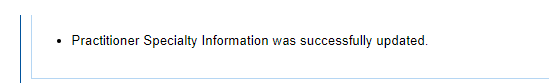
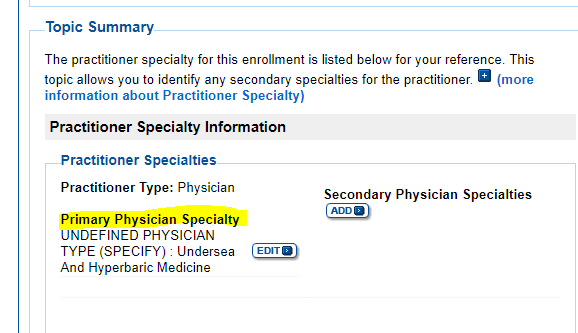
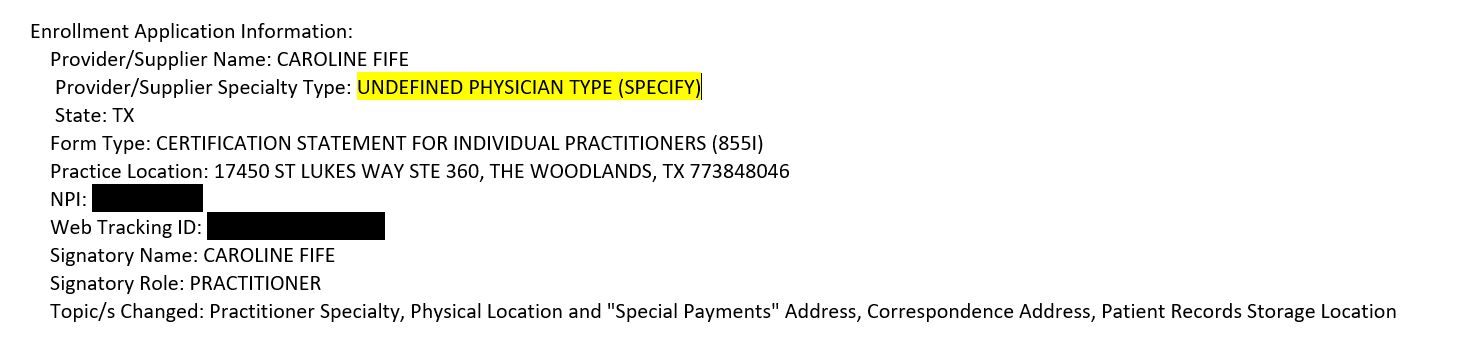
The CMS-855I and CMS-855O paper applications will be updated to reflect the new physician specialty but in the interim, providers should select the “Undefined physician type” option on the enrollment application and specify “Undersea and Hyperbaric Medicine” in the space provided. (See the screen captures below, which Kathryn was kind enough to provide! Unlike checking your data on Physician Compare, this process was relatively simple and did not take long.)
This is important – existing enrolled providers who want to update their specialty to reflect the new specialty must submit a change of information application to their Medicare Administrative Contractor (MAC) within 60 days of the January 7, 2019 implementation date which, by my unofficial read, would be by March 8, 2019. Information about this is provided in the MLN Matters article linked here.
You can get more information here:
- https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R309FM.pdf
- https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R4184CP.pdf
Visualizing the Complex patient
- https://carolinefifemd.com/2018/08/08/visualizing-the-complex-patient/
- https://carolinefifemd.com/2018/11/15/wound-cares-bermuda-triad/
- https://carolinefifemd.com/2018/11/13/visualizing-the-complex-patient-2/
- https://carolinefifemd.com/2018/08/29/visualizing-the-complex-patient-and-the-implications-for-cellular-products/

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.