In 1998, when I initiated a lymphedema program within a busy wound center, I had no idea what I was doing. I had been running the Memorial Hermann Wound Center in the Texas Medical Center for eight years by then. Women with post-mastectomy lymphedema began to call and ask me about obtaining treatment for their lymphedema. I would ask if they had a wound and when they answered “no,” I would politely say that we only treated wounds at the wound center. Thankfully, women on a mission are persistent. Eventually, I asked myself, “Well, where DO these women go to get treatment for cancer-related lymphedema?” The answer in 1998 in Houston was “nowhere.” I took myself to the National Lymphedema Network annual meeting and I purchased what was, at the time, about the only textbook available on lymphedema management, and I convinced the hospital to hire a part-time lymphedema therapist. I was not expecting to have many patients, particularly since (as usual) the hospital made no attempt to advertise that lymphedema therapy was available.
And then the floodgates opened
Entirely thanks to word of mouth and wonderful, persistent women, I soon needed six full-time lymphedema therapists to meet the demand for lymphedema services. In addition to post-mastectomy lymphedema patients, we saw men with prostate cancer-related lymphedema, and children (even newborns) with primary lymphedema. The scope and severity of the patients we treated was mind boggling. This evening I took a walk down memory lane, reviewing some of the presentations that the lymphedema therapists and I gave at national meetings over the 15 years of this huge program. Not only were we able to improve the lives of cancer survivors and children with primary lymphedema, the therapists enabled us to heal wounds we had not been able to heal before — because we were finally able to control local swelling.
It was divine timing that at the same time, Dr. Eva Sevick was looking for a clinical program with which to partner in the development of real-time lymphatic imaging. Prior to lymphatic imaging, I felt like I was practicing medicine in the Victorian era — with little understanding of the physiology of the disorder, and no way to image the disease to understand it better. When Dr. Sevick was able to give us pictures of the lymphatics and their function (or lack thereof), I knew what it must have felt like to see the first X-ray, the first MRI, or the first angiogram.
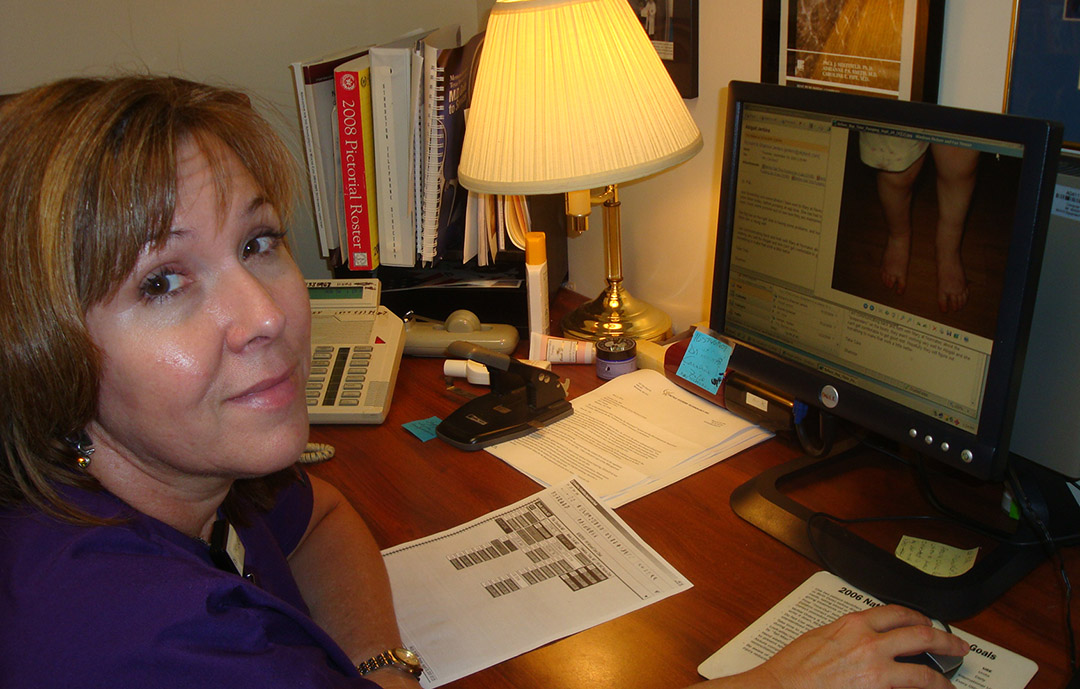
My point is that I knew absolutely NOTHING about lymphedema when I started the Memorial Hermann program. The lymphedema therapists (and the patients) were my teachers. I could fill a book with examples of the way these amazing therapists trained the wound center physicians. However, I think you should hear the story from one of them, my friend and colleague, Missy Baylor. (Here is a photo of Missy in 2009, doing “telemedicine” before anyone was talking about telemedicine, for a child with primary lymphedema.)
At the top of this post, you can see the amazing team (in masks, thanks to COVID, from left to right): Michelle Robles, Lisa Kinder, Susan Harrelson and Missy Baylor.
The Lymphedema Therapist: A Wound Physician’s Secret Weapon?
By Missy Baylor, OTR, LMT, CLT-LANA, CSWS
Occupational Therapists (OT) and Wound Care
The recent articles on lymphatic imaging and collaborative care in wound management prompted me to write about my experience as an Occupational Therapist who specializes in lymphedema therapy and wound care. I work in a wound and hyperbaric clinic, and feel I am a rare breed since most people don’t equate Occupational Therapy with wound care. In fact, some OTs may even be surprised to learn that the Occupational Therapy Profession Scope of Practice, Texas Administrative Code, Title 40, Part 12,§ 362.1 includes (section C):
“Interventions and procedures to promote or enhance safety and performance in activities of daily living (ADL), instrumental activities of daily living (IADL), education, work, play, leisure, and social participation, including: (xiii) Application of physical agent modalities, and use of a range of specific therapeutic procedures (such as wound care management; techniques to enhance sensory, perceptual, and cognitive processing; manual therapy techniques) to enhance performance skills.”
What do OTs actually do?
Occupational Therapists bring a different skill set to the field of wound care, because our focus is on helping people “participate in the things they want and need to do through the therapeutic use of everyday activities (occupations).” Unlike other professions, occupational therapy helps people function in all their environments (e.g., home, work, school, community) and addresses the physical, psychological, and cognitive aspects of their well-being through engagement in occupation.” Just for fun, ask ten different people (physicians included) what the difference is between physical therapists and occupational therapists, and chances are you will get ten different answers.
What do lymphedema therapists actually do?
Maybe we should start by asking what lymphedema is! Ask any physician how much time was spent in medical school on the lymphatic system or the treatment of lymphedema, and if they are honest, they will admit that they got very little training on this subject. It explains why patients with lymphedema typically see multiple doctors before finding one who can diagnose their lymphedema or make a referral to a lymphedema therapist. Admittedly, the standard occupational therapy curriculum does not include treatment of lymphedema and/or wound care. OTs who do obtain certification in lymphedema therapy would still benefit from a basic course in wound care because it is inevitable that a lymphedema patient will show up with a wound. I was most fortunate to get my feet wet (sometimes literally!) learning wound care under the tutelage of some of the very best hyperbaric and wound care physicians (Dr. Latisha Smith, Dr. Erik Maus and Dr. Fife). We had a very collaborative team where the doctors and nurses were always available to answer the therapists’ questions and assist us with complicated lymphedema/wound patients. The physicians learned as much from the therapists about lymphedema and manual lymphatic drainage as we learned about wound care from them.
Lymphedema Treatment
Lymphedema therapists spend 30 to 60 minutes “hands-on” with a patient to perform manual lymphatic drainage, usually up to three times a week for 2 – 3 weeks. The hands of an experienced therapist can discern changes in the affected tissues that are not visible to the naked eye. It is empowering to the therapist when a physician listens to their concerns. In the past, there was no diagnostic tool available to substantiate the therapists’ clinical instincts. But now there is a diagnostic tool, thanks to the decades-long work of Dr. Eva Sevick. When you see the images of dermal backflow on the ICG imaging of venous insufficiency and wounds, it makes perfect sense that manual lymphatic drainage would improve the lymphatic function of the affected area, thereby improving wound healing.
Clinical Examples of Collaborative Care with an OT
The tactile sensitivity developed from years of hands-on experience has helped me detect metastatic changes in several oncology patients. One of these was a lady with post-mastectomy lymphedema several years out from her cancer treatments, who arrived at her initial evaluation with her left shoulder elevated almost up to her ear. Besides having left arm and truncal lymphedema, she complained of pain in the neck and shoulder and she had limitations in shoulder range of motion (ROM). After successfully reducing her arm swelling and transitioning to the maintenance phase of self-care for her arm edema, she continued to present with lymphatic congestion and pain in her neck and shoulder. After several sessions with her, my “spidey-senses” tingled when I palpated this area or attempted passive range of motion (PROM). I encouraged her to follow up with her oncologist or PCP and suggested a referral to physical therapy for pain, weakness and ROM deficits. Even after negative report on radiographic imaging of her neck and shoulder and a course of physical therapy, she still had no relief. At my insistence, she followed up with her oncologist and diagnostic imaging detected a sarcoma, not related to her original breast cancer.
Another patient was referred for lower extremity lymphedema treatment in the context of pain, swelling and weeping from his posterior right ankle which had been present for 2 weeks. He had signs of venous disease on both legs (e.g. hyperpigmentation, hyperkeratosis, and edema) but he had very severe pitting edema of the right ankle and ankle pain at a level of 5 out of 10. When I palpated the right ankle, it was hot and felt “spongy.” His right calf was hard and fibrotic. It’s amazing how often, if you take a complete history, the patient will tell you what is wrong with them! He related that 20 years ago he fell from a ladder, was in a coma for 3 days and had a broken back, hip, and ankle. Over the ensuing two decades he had undergone more than 20 operations related to these injuries, including the placement of metal hardware in the right ankle. He had also suffered frequent episodes of cellulitis in the right lower extremity and at times had ankle pain so severe he was unable to walk. During his most recent exacerbation, he had gone to a local emergency room and was diagnosed with a sprained ankle and given crutches. Later a different physician diagnosed him with gout. Finally, a vascular surgeon recognized he had lymphedema and referred him for lymphedema therapy.
After one session with this patient, I was very suspicious that his problem was actually osteomyelitis. I was surprised that none of his physicians had considered this possibility, but perhaps no one took the time to get the whole story or to really listen to the patient [Fellow physicians, please take note! CF]. I contacted the referring vascular doctor and expressed my concerns that he might have a chronic infection, and I encouraged the patient to see his primary care physician and ask for an imaging study since he had never had an MRI of his ankle. He was eventually diagnosed with osteomyelitis, and the necessary surgery was performed. With his infection resolved, he no longer uses a cane, his skin integrity is greatly improved, and he now wears normal fitting shoes. He is very grateful that someone took the time to listen to his story.
Lymphedema is a complicated and mysterious disease, and the patients often have many co-morbid diseases. (See previous articles linked below about lymphedema and these challenging patients). Many physicians aren’t sure where to refer complex patients with swelling. Part of the problem is a shortage of certified lymphedema therapists. I believe every wound center should have a lymphedema therapist on site but there are a lot of regulatory and reimbursement barriers that have to be overcome. I hope that my passion in caring for lymphedema and wound patients will inspire other Occupational Therapists to become Certified Lymphedema Therapists and Certified Wound Specialists. OTs can be vital members of the multidisciplinary wound care team, and Lymphedema therapists can be the wound care practitioner’s secret weapon in the team approach to these challenging patients.
 The illustrious Sevick Imaging Team (from left to right) Melissa Aldrich, Grisseld Virtue, Susan Harrelson, Michelle Robles, John Rasmussen, Lisa Kinder, Eva Sevick and Rodney Morrow
The illustrious Sevick Imaging Team (from left to right) Melissa Aldrich, Grisseld Virtue, Susan Harrelson, Michelle Robles, John Rasmussen, Lisa Kinder, Eva Sevick and Rodney Morrow
Previous articles about lymphatic imaging and lymphedema:
- In case you missed it in 2017: A Taxonomy For Skin Disorders in Lymphedema Patients
- Wound Care’s “Bermuda Triad”
- Why my Blue Mondays are Happy
- If Success and Failure Look the Same, We Have a Problem
- The Inconvenient Truth in a Convenience Sample – the Prevalence of Lymphedema in a Wound Clinic
- 3 Patients with Lymphedema of the Hand – One of Them Has Open Wounds – Why?
- Visualizing the Relationship Between Venous Insufficiency and Lymphedema
- Arcanum Aqua – the Mysterious Water Problem of the Lower Extremities
- The Wound Whisperer – Lymphedema of the Plantar Foot
- Valentine’s Day Meets Venous Disease
- Near Infrared imaging of Venous Occlusion
- The Red Leg

Dr. Fife is a world renowned wound care physician dedicated to improving patient outcomes through quality driven care. Please visit my blog at CarolineFifeMD.com and my Youtube channel at https://www.youtube.com/c/carolinefifemd/videos
The opinions, comments, and content expressed or implied in my statements are solely my own and do not necessarily reflect the position or views of Intellicure or any of the boards on which I serve.




It’s helpful to know that a lymphedema therapy session can last for about an hour. A friend of mine is considering to undergo a certified lymphedema therapy soon because she is still experiencing some pain after an unfortunate car accident a few weeks ago. Perhaps she still has some tissues that need some recovering despite not looking injured from the outside.